Sarah: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families, and communities. I'm Sarah Hexem Hubbard with the Pennsylvania Nursing Workforce Coalition and the Executive Director of the National Nurse-Led Care Consortium.
This is part one of a special maternal health series. On this episode, we're going to hear from Miyah Davis about how she became a doula after being a client with the Philadelphia Nurse-Family Partnership here at NNCC. Nurse-Family Partnership is an evidence-based home visiting model that serves first-time parents from pregnancy until their child turns two. Home visiting programs aim to strengthen families by walking alongside new parents and empowering them to reach the goals that they choose for themselves and their children.
This past year, NNCC worked with the Maternity Care Coalition (MCC) and the Pettaway Pursuit Foundation to not only increase access to dual services for clients enrolled in home visiting services, but also connect parents who had graduated from our programs with the opportunity to become a doula. For those who don't know, a doula is someone who offers individualized, physical, emotional, and informational support to clients before, during, and after childbirth, though they're typically best known for supporting mothers in labor and delivery. Our guest, Miyah Davis, became a doula at the end of 2024 and first connected with the Philadelphia Nurse-Family Partnership in 2019 when she was pregnant with her first child.
In addition to being a doula in her spare time, Miyah works a full-time job and is raising children with her husband.
Miyah, welcome to At the Core of Care.
Miyah: Hello. Thank you for having me.
Sarah: First off, congratulations to you on becoming a doula.
Miyah: Thank you so much. Thank you. Thank you.
Sarah: So could you tell us the story of how and why you decided to become a doula?
Miyah: I was working at a nursing home and I don't know, I just was feeling like this isn't necessarily my calling, like I want to go somewhere where life is just beginning, you know? But I didn't want to go to like nursing school. I didn't want to become a CNA or anything like that. And I also was like kind of in the middle of a identity crisis. 'Cause I really didn't know who I was outside of being a mother and a wife. So I didn't know what I wanted to do or where I wanted to go. I just knew that I didn't want to be in geriatric care anymore.
And it might sound a little cliche, but I did pray on it very, very hard. And it's like, right after I got done praying, I got a text and it was like a automated text that said, you know, Nurse-Family Partnership’s graduates are being granted scholarships to be able to become a doula. So I said, oh, thank you. God, you're, you're quick. That was fast. And I, um, I signed up with no questions asked. I didn't think twice about it and I just applied.
Sarah: Thank you for your interest and stepping up. So from what I understand, you're a doula right now for, is it eight clients?
Miyah: Yes.
Sarah: Yeah, so at what point during the client's pregnancy do you get matched up? What does the process look like?
Miyah: So every Monday, MCC sends a mass email to every doula. It's called a client match list, and we get to click the match list, and then we search through.
They don't have like their names or anything like that. It's like numbers and then it have their due date or where they're having their baby, and it has in quotations, if they have like a specific preference. You just go based off who you think is the best fit for you. One of my recent clients, she specifically says she wanted a Muslim doula, so I had asked to match with her, and in which I did, and we just had our first visit yesterday.
She is so sweet. She's so nice. But MCC doesn't allow you to have clients that like overlap, like the due dates overlap. Like if they're within the same timeframe or the same month, they'll tell you like, oh no, I don't think you should match with this one, because the due dates are too close together. So pretty much I have a client due almost every month this year, except for I think September, November, and December.
Sarah: Busy.
Miyah: Yeah.
Sarah: And how often do you interact with clients sort of leading up to labor and delivery?
Miyah: MCC grants us five visits, but I still talk to my clients pretty much every single day. I had one client that I actually was texting before I came here. Um, we talk like we're girlfriends, like, and we, we, we just matched with each other last week.
We keep in contact a lot. We have to spread our visits out, but we see each other a lot. I have a couple clients who I see outside of the five required visits. 'Cause I just feel like, sometimes you need that extra support. And everything doesn't have to be something that you're getting paid for. It doesn't have to be something that you have to be reimbursed for. Like I just do a couple visits outside of that from the heart and stuff like that.
Sarah: And are the five visits in person or telehealth, like what does that look like?
Miyah: It can be either in person or virtual. Usually my first visit, after the intake, is usually virtual. And you know, that just gives us like a little warm welcome. You know, we finally get to see each other face to face, I guess, through the phone.
And then after that we do in-person visits. But the birth is considered a visit as well, so we gotta make it stretch between birth and prenatal and postpartum.
Sarah: Could be a really long visit.
Miyah: Yes.
Sarah: So what types of conversations do you have with clients?
Miyah: During the intake, I kind of like try to break the ice. So if they have previous children, I typically ask for your previous deliveries, vaginal C-section. Are you going for a vbac? I like to ask about their past experiences and how they're juggling with being pregnant and having children.
But if they're like a first-time mom, I like to ask them like what their confidence level is and what exact support do they want from me.
Most of the times you have to ask them, do you even know what a doula is? Because a lot of them just sign up because they were asked. And they just like, yeah, just sign me up, sign me up. And then once I reach out, they're like, well, I don't even know what a doula is. So you definitely have to lead with that in most cases.
But I have a client now who, she did her research. She has an older child already, but she didn't have a doula with her oldest child, and she's trying to have like a VBAC or something now. She looked it up, she searched up what a doula was and what we offer. So she was telling me like. She was informing me, and I was like, okay, I don't gotta do, I don't have to explain too much here. She already knew what she wanted
Sarah: And I think it's a good call out. I gave a very brief definition of a doula, you know, in the start here, but I think it would be helpful, like, how do you explain that? What is a doula?
Miyah: So when someone asks me, what's the doula, I tell them, I'm there to advocate for you if you can't advocate for yourself. I'm there to make sure that your birth plan goes according to plan, with also being flexible to changes.
I also tell 'em that I'm there for emotional and physical support. I also have to let it be known, I'm not a midwife. I do not catch the baby. I do not take your vitals. I do not have a heartbeat. doppler, I don't do water births. I also have to explain that. But you know, I just tell 'em that I'm their plus one. I'm the companion of their companion. Because then you have some that have partners and stuff like that. I'm not here to replace your partner. I'm not here to be there instead of your partner. I'm just there to assist everyone and to make sure that the baby comes out safely and everybody's happy and healthy.
Sarah: So what was it like attending the first birth with one of your clients?
Miyah: My first client, she was going through like a sickle cell crisis and I was at my full-time job actually. Actually, she went in a lot earlier than she was supposed to, she had to stay in as an inpatient. And I let my job know. I'm like, listen, when my client says that she's six centimeters, I'm outta here. Like you, you, you knew I was a doula when I first signed up for this place. If she calls me, I'm out the door. I. But the labor process was going pretty slow. I work 12-hour shifts, so I'm like, I hope we can get through this day.
But with my first birth, it was more virtual. She was in a lot of pain. So I mainly spoke to her mother, and her mother was very informative. She was very communicative. She reached out to me every time she needed to know something, or if it was something that she was confused about. She kept me updated throughout the entire process, which means a lot in the doula world because sometimes you don't get updated. Sometimes you don't even know the baby's here until two days after the baby is born.
So I liked that her mom kept me involved, and of course I checked in every two hours. She was in a lot of pain, so her mom wanted to know how to help her with pain management. So I sent her different videos. I told her how to do the massages and I told her to let my client know how to like flip over and do different positions to like help manage her pain.
She tried to go as natural as she could for as long as she could, and she did a very, very good job. And her mom being there definitely made it like a plus one.
And, um. She made it through my whole shift without reaching six centimeters. It was about, I want to say 10:00 PM and she was like, oh, I'm four centimeters now. And I was like, okay. I am going to give me a little nap in and then I'll, I'll be there.
So I don't know how to drive, but my husband drives me everywhere. I'm, you know, they say passenger princess. I'm a passenger queen because I never get in the driver's seat. So, um, I'm telling him like, babe, we're on call. Make sure my doula bag is in the trunk, and if I say, get up. Get up.
So I went and took a nap, but he stayed up and she called me at like 11 and was like, I'm seven centimeters, seven. Oh my God. I had to jump out of the bed. I'm like, babe, she's seven centimeters. He running up the, you would think it was me that was having the baby like we got in the car.
When I tell you he was speeding down the street, you would've thought that it was me in labor, like he was making sure that I got there. We pulled up, I jumped out, I went in through the door. They was like, oh, you're the doula. You can go right upstairs.” It felt good. It felt like first class.
I went right up the steps and I walked in and I'm like, hello everybody, and there's all these doctors around her and I literally went, hello, everybody. And the baby was coming out. I’m like, oh my god. I feel like I done miss the whole thing, like the baby's here. Now, I'm like, well, at least I was, you know, here to see the baby come out. And I immediately rushed into action. I rubbed her head, I rubbed her arms. I watched her push out her placenta. She let everyone in the room like her mom and her dad ended up showing up as well.
It was a beautiful moment and she wanted to breastfeed and I told her about this video that was showed to us in the doula program, and it's basically saying how your baby can latch themselves and all you have to do is not wash off their hands and not wash off the breast because the hands have like a amniotic fluid smell and the breasts smell similar and the baby will like rest for a little bit, but then they'll gnaw on their hands a little bit and then locate the breast.
So I sent her the video so she was all for it. Soon as they pulled him out, she's like, don't wipe his hands. Don't wipe his hand. So I'm like, okay, he's not going to wipe his hand. She's still going to do it. Her dad cut the umbilical cord, they laid the baby down on her chest, and he was resting for a little bit.
You could tell he was very tired. He didn't cry. That was the first time I ever seen a baby come out without crying. He was so content, she was so calm. The baby was calm, the music was playing. It was just like very beautiful and it just felt so natural.
The baby was laying on her chest. He slept for like a good 10 to 15 minutes. Then he got up and started to gnaw on those fingers and she's like, let's lift him up a little bit. So she lift him up a little bit and he went searching for the nipple and I'm like, oh my God, he's doing it. So I'm in there jumping up and down and I'm cheering and I'm clapping, and. She's like, oh my gosh, he's going to find it.
And he did. He found it, but he couldn't like necessarily like latch on that much 'cause it wasn't really flowing. Because you know, right after birth it doesn't flow like that. So he would latch, then he would let go, and then he would gnaw his fingers and then he'll go back and latch again because he’s like, wait, I, I think I'm here, but I'm not sure.
But she remained very calm. She was very patient. And I kept telling her that she was doing a good job, kept encouraging her and giving her the nice words of affirmation. Her mom was also there, crying. I started crying because it was a beautiful thing for me. And I'm like, I never witnessed nothing like this before. And I had three kids. I need a redo.
Like, it was so nice. Um. And then she did skin-to-skin for two hours. I stayed for after the first feed and they delayed the weigh-in and stuff like that. She got up, used the bathroom quick. She bounced back fast, like I commend her. She did the thing. She did it. It was a good experience.
I got there right when the baby came out. The baby came out at 12:12 and I left at like 2:30 and I had to go to work at 8:00 AM.
Sarah: It's a good thing you got that nap in.
Miyah: Yes.
Sarah: So have you attended any other births since that first one?
Miyah: No, not yet. But I do have a client now that's being induced. So, I already let the job know once she six centimeters, gotta go.
And my husband already knows to be on standby, had the doula bag in the trunk because when I say Let's go it, it's time to go.
Sarah: So, during your first birth, what was your experience like? Did you have a doula or other birthing assistants?
Miyah: Well, with my first birth, I did have a doula. I'm not going to lie, I had a doula. But I wasn't aware that you could have preferences with your doulas.
And so I was a first time mom and my doula didn't have any kids, and we were the same age, and I was 20 at the time. So, you know, she was out having a ball. So.
You know what? My Nurse-Family Partnership nurse, she told me to look at the bright side of the situation. 'cause I complained to her about the fact that she didn't have kids and the fact that she doesn't have her own experience.
And at that time, you know, I was like, I don't know, like what can she teach me? And she was like, maybe you two can learn together. And I was like, you know what? Maybe we can. So I stay very optimistic about the situation after my nurse telling me that. And we got along good, but I didn't call her to the birth because I feel like it, probably was the hormones, but I was a little upset.
Because she went to, she went on a trip a week before my due date, and she was supposed to have like a visit two to three days after she came back home. And she just was like, “Oh no, I'm sick.” And then that's when we were supposed to do it three days after that. “Oh no, this came up.”
So it's like, you know, the baby is about to come soon and it's like, I can't reach you. You're not answering the phone. And I just was like, you know what? Okay. And my son was due January 14th, but I got induced January 6th. So I just said, I'm just going to just leave it where it's at. So I didn't call her. I probably should have.
After experiencing what I did during the labor process, I do regret not calling her. I should have called her so I could have that advocacy, so that I could have someone who was informative, even though I did learn a lot from her and my nurse, I feel like I should have called her. But she was there through my postpartum.
She went with me, um, up to the child support court and everything. So she was supportive in that aspect. Like after the baby was born, she went with me to the WIC office and she got my WIC for me a couple times as well. She was very, very helpful for the postpartum period. But no, I didn't call her for my birth.
But I had a doula for my other two births, it was the same doula. I called her again once I got pregnant with my third one. I called her again with my second one. I don't remember what agency I met her throug. 'cause none of my doulas were like through MCC. They were just something that my insurance referred me to.
But I met my second doula, and she was Black, she was Muslim, and she had kids and she was a wife. So I'm like, perfect. This is the one for me. This is for me.
She was very stern. She was very serious about her job and you could tell that she loved it. And she made me feel comfortable. She made me feel heard. She was there a lot through like emotional support. She was very supportive. And, um, when she came to my second birth, she answered every time I called her, if I called at 2:00 AM she answered the phone. If I called at 1:00 AM she answered the phone. She was on call. She was ready.
But she ended up missing when the baby came out. So when she came in the room, when my water broke, I started pushing. I wasn't supposed to, but I was pushing and she's in the room. My husband's in the room. My husband's on FaceTime with my mom and my mom's screen recording because we wanted to have a video when the baby came out.
So she comes in, she's putting her bag down. Everybody's talking and I'm just sitting in the bed with my legs gaffed open, looking around in complete agony and pain. Because I had the epidural, but. all my contractions went to my behind, so that's a pain I wouldn't wish on my worst enemy. So I'm in there in agony while everybody's just scrambling around.
Now it's time to push. So I push the first time and I'm, my jaw was already pushing when I wasn't supposed to, so I'm pushing, and his head instantly pops out. Mind you, my husband's on FaceTime. He's talking to my mom. She's in the corner putting her stuff away and pulling stuff out, and then. My husband has the camera on me this time, and he's ready.
And then she says something to my husband, which made him turn around, and then he turned back around and the baby was on my chest. So he missed it. And she missed it. They were like. Wait, what? When did the baby come out? My mom's on FaceTime. Like, wait, hold up, hold up, go back, put him back in. Do it over.
They're like, oh my gosh. Like when did you have the baby? I'm like, so y'all standing here? Neither one of you seen it. My husband like, no. She called me. I turned around, turned back around and he was on your chest and she like, I'm talking to you. It was, it was crazy. And um.
My third pregnancy with my daughter, I ended up having an emergency C-section, so she was on call, but she didn't come up due to the simple fact that you can only have one person in the room. But she did help me with like my postpartum care and stuff like that after that. So if I was to get pregnant again, I would most likely call her back again.
Sarah: I mean, anything involving birth is difficult to time, but I think that that story was next level on just how to the moment it can be.
So in your own journey to become a mother, clearly have a lot of experience and experience working with doulas, how did that experience shape the decision to become a doula?
Miyah: Well being though I had two different kinds of doulas. I had the experience of what kind of doula I kind of want to be like, and I also had the experience of a doula who I kind of don't want to be like. But she was still helpful in a way. And I do still appreciate her. Being though I had like a taste of both of those.
It inspired me to be someone who's consistent 'cause that's what a lot of the clients need. They need someone that's consistent and reliable and knowledgeable. Because a lot of clients who have like age gaps with their children or no children at all, they tend to rely on the elders in their family. And time's changed. Time has changed. Tom's isn't the same as 1999 when I was born, so you can't really always rely on Mama Shirley or Aunt Stephanie to get you through your labor. So it definitely inspired me to be for other people, what I had for myself.
I love working with people. I love babies. I love being supportive. I love being that person that someone can call on in their time of need and my experiences I had that I had someone that was there when I needed them. My first doula, like I said, we used to get my WIC for me, my other doula, she was there for a lot of my emotional support and a lot throughout my, um, prenatal and postpartum.
And I just wanted to be that for someone else. I just wanted to be there and always be there. And even if you feel like you don't have anyone, you got Maya.
Sarah: And I understand you had a, a really close relationship with your home visiting nurse. So how did that help with your first pregnancy? What was that like?
Miyah: She was amazing. I'm going to try not to cry 'cause I always get emotional when I talk about her because she was like the only consistent person in my life at that time. I went through a lot during my first pregnancy. My first child isn't by my husband. So I was in kind of a, like a toxic situation. And then um, I was going through a lot of drama at home with like my mom and my family and stuff like that.
I just feel like when you pregnant people test you 'cause they know you can't really do too much. So I just felt like I was being tested a lot and I felt abandoned by everybody but my nurse. It didn't matter where I was 'cause for a little while I was homeless. I didn't have anywhere to go. I was just house hopping between like friends and family members and stuff like that.
So for a little while, I really didn't have any stable place and I didn't know where I was going to go, what I was going to do. And, uh, my nurse was there. She was there. It didn't matter if I was in Allegheny on this week and y the next week, I could have been in Southwest the following week.
It didn't matter where I was. She was there. She didn't complain. She didn't seem frustrated. She didn't make it seem like I was a burden or anything like that or inconveniencing her. She was always a phone call away if she was going to be out or go on vacation or something like that. She always let me know ahead of time and it was still a way for me to reach her even though she would be on vacation.
I just felt like I owed it to her to be in a better position by the time my child reached two. I just felt like I had to be in a better position 'cause I felt like I would've failed her if she didn't leave knowing that I was okay. Like I felt like I would've failed her had I not done that. So I had to push myself.
Sarah: Well, I won't speak on behalf of your nurse, but I do know your nurse and I know that she, you know, thinks the world of you, um, and there's not a thing you could have done that would've made her question anything about your success. And my understanding is that you've also maintained a relationship.
Miyah: Mm-hmm. Yes.
Sarah: So that probably helped with getting a text a few years later.
Miyah: Yeah.
Sarah: Um, take, taking a risk on a, on a doula opportunity.
Miyah: Yes. Yes. I was just like, oh, did my nurse put my name on that, um, on that list because it was kind of crazy. But yes, it was amazing. And when we did the interview for MCC, it was a lot of us in this Zoom video. It was over 75 people. 'cause I remember seeing a bunch of little bubbles at the bottom and then it says 75 plus. So it was a lot of competition and I'm just like, well dang, they might not even pick me because there's so many people here. They asked about, you know, availability and everything like that and if you'll be able to travel back and forth.
I didn't know if I was going to be able to travel. And then the job that I was working at before the nursing home, it was very demanding. It was taking up majority of my time, like I barely even saw my kids and it was hard to even get a day off there. So I had to figure out how I was going to be able to have off on Tuesdays and Wednesdays to even be able to go to class.
So I ended up adjusting my schedule at the job. They allowed me to switch my days, which meant I was going to be there a lot more due to that. But. It worked out and I got it done thanks to my husband and thanks to my brother, because when my husband couldn't do it, my brother picked up the slack. So I did have a nice village behind me while I was in the MCC course.
Sarah: So reflecting on your own experience as a first-time parent, and even how you were able to connect with doulas in your own experience. Now you are a doula. How do you think about access to maternal healthcare and support in birthing?
Miyah: I think the access, I don't think it's fair in a lot of cases because for me, I got my doulas through my insurance.
Not a lot of people have insurance and sometimes some doulas rather have it out of pocket and the. Prices are ridiculous. Like one of my clients said one of her friends is a doula and wanted $2,000 for her to be her doula, which, you know, you pay what you feel like you're worth, you know?
But, um. Sometimes I feel like it can be very unfair and I feel like there's not enough promotion on it. If you're not going to a doctor's appointment or if you're not asking for resources, they're not throwing in your face, here's a doula. You have to show like you want something like that or have something going on to where people will offer doula services to you.
Like when my insurance offered it to me, they were just like, are you open to resources? Say for instance I had to said no, I would've never knew, like. Or say for instance I had to been one of those that just be like, uh, I don't, I don't really care for resources. You know? Sometimes some people aren't educated on it, so I feel like it's a little unfair.
I feel like the access to having a doula and that support, it definitely should be broadcasted more, and it definitely should have easier access, and it definitely should be something that people know in the beginning and not just if they need help.
Sarah: From your perspective, what do you think might benefit families more during the prenatal and postnatal stages? What other resources would be helpful?
Miyah: Lactation classes because nowadays breastfeeding is the thing, like everybody wants to breastfeed. Everybody understands the importance of breastfeeding, and I wish that I knew the importance of breastfeeding when I had my kids. My oldest son didn't get a drop because my stepmom and my father kind of scared me out of breastfeeding. They kind of told me I wouldn't have support if I breastfed. Second born I breastfed him for a little while, but it was kind of uncomfortable because his mouth was a little too small, so we had to use the shield and I didn't really do good with timing when to feed him.
Now I did breastfeed my daughter. About two weeks after she was born. I breastfed her for like a month until I just was like, Hmm, I'm tired of breastfeeding, I'm tired of pumping and I wasn't getting enough. And then she was like cluster feeding a lot. I wasn't really educated on that.
And you know, when you have the baby and they're trying to tell you the importance of breastfeeding and you got a baby in your arms, or if you got two toddlers running around the doctor's office, you ain't trying to hear that. I didn't want to hear anything about that. They were telling me how to eat and what to eat while the baby's crying and screaming.
It was overwhelming. So I feel like during like the prenatal stages, lactation should definitely be installed in the parents ahead of time so that they can mentally prepare themselves and have the patience somewhat when the baby comes.
Sarah: I think that's a great point in terms of the prenatal care, and I'm always really impressed when our pregnant clients come to our lactation support groups and I'm like, oh man, I wish I had thought of that.
I have twins and after they were born I needed a transfusion and I still remember. So when you have twins, they really push pumping like immediately 'cause they want to get your supply up. And they rolled in the giant hospital pump and I'm there like hooked up to the blood. It's like roll on out.
And I just, I still remember that so clearly because yeah, there's so much going on, especially in a hospital setting, people coming in and out, and it can be difficult to receive that information.
And breastfeeding is hard. It's hard. Every baby's different. Every mom's different. Um, so I hear you on the being as prepared as possible and knowing that you can't possibly be prepared for everything.
So anything else that you think would be helpful in advance?
Miyah: I also feel like birthing classes are important because a lot of my clients tend to look at other people's experiences and try to put their selves in that person's shoes. Just because that person was in labor for 48 hours doesn't mean you're going to be in labor for 48 hours. Just because that person said that the contractions hurt them, doesn't mean it's going to hurt you.
Everybody automatically thinks, oh, I'm with the epidural. You didn't even feel a contraction yet. Like you don't even know your pain tolerance in that aspect. So I feel like that should also be something that's pushed upon.
Sarah: Absolutely. That makes a lot of sense. So before we end our conversation for today, are there any final thoughts you'd like to share? Anything that you want to make sure that our listeners hear?
Miyah: I would like to say, you are doing a great job to all my mothers out there, all my birth people out there, you're doing a great job.
Don't ever get discouraged if your birth doesn't go according to what you planned or written down. Everything happens for a reason. You're a great mother. You're a great parent. You're a good provider.
Always take some time out for yourself. Self-care is definitely important. Sometimes we lose ourselves and we tend to lose our identities when we are parents or become parents.
Your child is in the best hands and, like my nurse at home nurse used to tell me, nobody loves your child like you can. Nobody can do for your child the way that you do. And to the partners of the birthing people, you are amazing. You are just as important. You matter as well. And we are thankful for you, for your support, for your helping hand, for you also being a voice to the one that's bringing the baby in the world. 'Cause we tend to forget about the people that support and my, know, my husband was a great support. So, yeah.
Sarah: Miyah, thank you so much for responding to that text, for going through the program, for entering this amazing, crazy world of doula care and certainly for sitting down with us today at At the Core of Care.
Miyah: No problem. Thank you so much for having me. Thank you. Thank you. I hope my words touch some people.
Sarah: Special thanks to Maya Davis for joining us. In part two of this series, we will talk about policies surrounding doula care and opportunities for the future. You can find our most current and past episodes of At the Core of Care, wherever you get your podcasts, or at panursingworkforce.org.
For more information about upcoming webinars and trainings for nurses to obtain continuing education credits, log on to panursingworkforce.org.
On social media, you can stay up to date with us through our handles @nurseledcare and @PA Nursing Workforce. At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder. I'm Sarah Hexem Hubbard of the Pennsylvania Nursing Workforce Coalition and the National Nurse-led Care Consortium.
Thanks for joining us.
SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families, and communities. I'm Sarah Hexem Hubbard with the Pennsylvania Nursing Workforce Coalition and the Executive Director of the National Nurse-Led Care Consortium.
On this episode, we're gonna talk about the latest trends around rural health with Lisa Davis. Lisa is the director of the federally funded Pennsylvania Office of Rural Health. She is also an Outreach Associate Professor of Health Policy and Administration at Penn State University Park. As the director of Pennsylvania's Office of Rural Health, Lisa makes sure that the state office exceeds its federal mission of being a source of networking, coordination, and technical assistance to advance rural health care delivery.
She serves on various local, state, and national boards focused on rural health and is a member of the Pennsylvania Nursing Workforce Coalition's Nurse Diversity Council.
Lisa, welcome to At the Core of Care.
LISA: Thank you so much for having me.
SARAH: So we have known each other for a while now. But I don't know what drew you to the issue of rural health to begin with, and you have devoted your career to this area of healthcare.
LISA: Well, I have to tell you. I actually did not know that there was a career in rural health. Penn State had started the Pennsylvania Office of Rural Health when I was in graduate school many, many years ago, and I interviewed for a position as the first full-time staff person, which was the outreach coordinator position at the time, and I absolutely fell in love with rural health.
I had always focused on the sort of un and underinsured and very vulnerable populations, and also wanted very much to get into policy. And so this really combined both of those passions. And I realized that I had not ever anticipated that I would meet a group of people in communities across the state and nationally who were so incredibly smart, talented, knowledgeable, and passionate about the work that we were doing, and they're also a tremendous amount of fun.
And so the rural health community is pretty small across the country, so we're a pretty tight-knit group. And I find that what we're doing is absolutely essential since Pennsylvania is such a rural state.
SARAH: Yeah. And so after Texas and North Carolina, Pennsylvania has the third biggest rural population.
LISA: So correct.
SARAH: Curious if you could share a little bit about the concept of rurality, how that's defined, and why that matters.
LISA: Well, it matters a great deal especially if you are a facility that can be reimbursed at a particular level or be designated as a particular kind of facility. Same with a clinic, if it's not in a federally designated rural area. So I can tell you that at the federal level, there's probably no less than 40 different definitions of rural. And so, it's a bit challenging. You know, Department of Ag has one, Education has one, and so on.
We focus on the US Census Bureau and the Office of Management and Budget, and also a definition that was developed solely to focus on rural because all the other definitions sort of treat rural as whatever is outside of metropolitan or sort of a populated area. So the Rural-Urban Commuting Area, otherwise known as RUCA, was developed so that we would have a much clearer definition of what is rural, what is not rural, what's urban, and what is non-urban.
So, essentially, there is no straightforward definition. I wish I could tell you it is X and that is it. But a definition of rural really depends on if you have a population of anywhere between 5,000 and below or 5,000 up to 10,000 that is not contiguous to a metropolitan or urbanized area. So it really does need to be geographically isolated, and not be part of what's considered to be a metropolitan statistical area.
So we have counties in Pennsylvania that have more four-legged than two-legged creatures, that have no hospitals, very few primary care clinics or dental clinics and really essentially are what you would consider to be very, very rural. But, one county I'm thinking of a particular, is located inside a large metropolitan statistical area because everyone in that county empties out into another county during the day to go to work, and that commuting for work is considered to be a proxy for commuting for other goods and services like healthcare.
But, what I can tell you, is that Pennsylvania has 67 counties and 48 of them are considered to be rural. And up until the 2000 census, we were the most rural state in the nation. So when I would talk with my colleagues from Wyoming and Montana, and so on, when they would say, you're not rural. But they’re frontier, which is a very different definition. And we have maybe, I think two frontier communities in Pennsylvania.
But in the 2000 census, the US Census Bureau snuck in a sort of a mid-level definition called micropolitan. And so a lot of our folks that were in rural communities now we're considered to be micropolitan. But we're now number three. And of course, I still think we're number one.
SARAH: And for those who lost track in all of those different definitions, I always remember how Lisa described it to me maybe 10 years ago of, you know, Pennsylvania people think about the rural ‘T’ and really it's the rural ‘J.’ And so for those that are familiar with Pennsylvania, you have urban centers, Philadelphia and Pittsburgh, and then quite a lot of the center top and then that little curve at the bottom of the state that fit that definition of rurality.
So according to CDC and, many other sources, rural residents face many healthcare challenges. You know, most specifically I think, less access to specialized medical care and emergency services. But really a variety of things. Can you give us an overview of some of the unique factors that
LISA: Yes. So, when we talk about rural healthcare challenges, we talk about it under an overall rubric of access. And that is access to healthcare providers, including clinicians, and also facilities. Challenges with payment mechanisms, so how one pays for one's healthcare.
And then the third is the infrastructure, which is really the transportation, the geography, and high-speed internet. So when we look at providers, in general, we see that we have far fewer primary care providers in rural communities than we do in urban areas. That is across every single discipline: primary care, specialized care psychiatrists, nurse practitioners, physician assistants, dentists, dental hygienists, and so on.
So, in Pennsylvania, about 23% of the population lives in areas that are designated as rural. And so we're talking about a very large part of Pennsylvania. You know, as you were saying, we have the rural T and the world J. We also have a line that sort of goes across the northern tier that also connects very rural areas that sort of falls outside of being a specific letter in the alphabet.
So we have a lot of geography to cover. So having access to primary care is essential. That's the way people enter the healthcare delivery system. And we do have a really robust system of federally qualified health centers, federally qualified health center lookalikes, and rural health clinics.
And that is enormously helpful. But there are still areas in this state where it's very challenging to be able to access primary care services. Then when you begin to move towards specialized care, especially things like mental and behavioral health services or psychiatric services or maternity care, which I do want to talk about here in a second.
There are significant challenges. We also are seeing that across the state, even though we do have a lot of primary care clinics, we have, depending upon which definition of rural you are using, we have anywhere between 48 to 60 small rural hospitals. That's not very many hospitals to cover the entire state.
The state has 150 general acute care hospitals. So if only 60 of those are in rural communities, you can imagine how many places there are in the state that have no hospitals or have very limited access.
In fact, we have nine counties in Pennsylvania that do not have a hospital, and that becomes a real challenge because the hospital, in addition to the primary care services, is the center of healthcare for a community. It is where people go for emergency care. It's where they go for a whole wide array of primary care services for, you know, broken bones and the flu and all sorts of things, pneumonia and so on; diabetes care, all kinds of chronic healthcare conditions.
And if it's challenging to get to your hospital, that can really significantly interfere with your ability to be able to get the care that you need. The state has something called 17 Critical access hospitals, which are very small, very rural hospitals that are geographically isolated. And if they convert to designation as a critical access hospital, they get enhanced reimbursement through Medicare and also through Medicaid.
And then we have 70 rural health clinics, which from the naked eye look very much like a general primary care center. But they receive their designation as a rural health clinic where they do not need to have the direct oversight of a physician that other kinds of primary care clinics have.
And that is in recognition that it is so challenging to attract and retain healthcare providers in rural areas. So, rural health clinics are led by nurse practitioners. So those are just some of the issues that I can talk about in terms of facilities. We could spend an entire semester talking about it.
But the other is, when we talk about the types of individuals who are living in rural communities. Now, what I'm about to say is a complete generalization, but for the most part, rural residents tend to be older, sicker, and less financially advantaged than their urban counterparts.
They tend to have higher rates of chronic health conditions, such as cardiovascular disease and diabetes, and complications from stroke. They may or may not have full-time employment through an employer that offers healthcare insurance. And if they offer insurance, it may be a very narrow type of policy that may not cover dependents.
So we see a higher reliance in rural communities on the public insurance programs, Medicare and Medicaid, and CHIP, for access to healthcare and insurance coverage. For the most part, those tend to reimburse at a lower cost than private insurers.
Sarah: So what you're describing, especially, you know, looking at nine counties that don't even have hospitals. But also when you were speaking about primary care and the different types of providers that we see, to what extent has the makeup of healthcare delivery changed in your time at the Office of Rural Health?
LISA: I think here in the state one way that it has changed significantly is that Pennsylvania, I think, is one of the leaders across the country in consolidation of healthcare providers. So we have several very large healthcare systems that have essentially… not gobbled up, I don't mean that in a negative way, but they have purchased these small rural hospitals. And one of the challenges that we find with that and that we try, and do a great deal of education about, is that purchasing a small rural hospital is not just a way to bring additional patients into the tertiary care facility. In rural communities, the local hospital is a part of the fabric of the community, and we always encourage large healthcare delivery systems to be able to invest in their communities.
So that's been one change. The other big change that came about was in 2010 when the Affordable Care Act was signed. And that, of course, essentially changed so much because we saw that there were no longer restrictions on preexisting conditions. And we saw that individuals could be insured up to age 26. And we also saw the establishment of the federal, and now we have the state-based, marketplaces. And another big component of that really was a big impact across the country and here in the state, was Medicaid expansion. And that, I think, was a boon for Pennsylvania because the way that the Medicaid program is set up, it's a federal, state program. And so the federal government reimburses the state for a particular percentage of the amount that they spend on Medicaid Under the Affordable Care Act any new patients who came into Medicaid after the ACA was passed as part of the Medicaid expansion, the federal government would pay the states 100% of that cost. So it was advantageous for the state.
The other piece that was very advantageous for that was that now individuals who no longer had a way to pay for healthcare could pay for healthcare so that when they went to the hospital or the primary care clinic, they had a way to reimburse the clinics and the hospitals for that time. And then, you know, another really important piece that often doesn't get talked about, is that patients have access to care. And that is the number one predictor of whether or not someone will utilize care and potentially be healthier. So I would say that those are the two biggest things that I have seen since I came in.
SARAH: I loved how you described that with hospitals really being core to the communities that they're serving, you know, and there's so much of the local economy that is dependent on the healthcare sector. I mean that's true of all counties, urban, rural, and everything between. And rural hospitals in particular have experienced consolidation, and many closing over the last several years.
So recognizing the impact that you've seen from those closures and also the impact of access to public insurance for rural Pennsylvanians, what are some of the potential impacts for rural care in some of the conversations happening right now related to Medicaid?
LISA: Well, because Medicaid is a large pair of healthcare here in the state, especially labor and delivery, and also long-term care. Medicaid pays for 59% of all long-term care here in the state. If there are changes to Medicaid, we will absolutely see individuals who will lose their insurance coverage. And the idea is to implement work requirements. Many who are on Medicaid already are working. They just happen to be working for companies that do not provide health insurance. So they may be working, let's say 20, 30, 40 hours a week, but they're on Medicaid. So they obviously will not be required to have work requirements because they are working.
But for those who are not employed and who must go out and search for work. The question is, where are they going to go look for work? And how will they get there? If there's no car, we have very few public transportation systems in rural Pennsylvania, we have a couple, but they're not robust. It's not like being in Philadelphia or being in Pittsburgh. So those are some of these challenges. How will people get there?
What kinds of jobs are available? Because we have a really low unemployment rate right now in Pennsylvania, and we also know that during COVID, we lost hospital and clinic employees because they were able to go to positions at convenience stores or other kinds of jobs like that where they made essentially the same money, but they didn't have to do things like, worry about getting Covid or having to deal with irate patients and so on. So I think there's a real concern about that, and if that should happen, then all hospitals, including rural hospitals, will see an uptick in the number of uncompensated care that they provide because all community hospitals, all 501C3 hospitals, have to provide care regardless of a patient's ability to pay.
So that's going to be an issue that we're going to have to address. The other is if the subsidies for the health insurance marketplace should end, we are looking at thousands and thousands of individuals in Pennsylvania who will likely lose insurance because they are not able to afford the full premium. So we're now going to be looking at additional individuals who are uninsured.
SARAH: So for more than 40 years, every state has had some type of rural health entity. And the mission is really all-encompassing. I think that you had once stated that your job is to do everything, everything related to rural health.
So can you give a little sense of your reach in Pennsylvania, some of the key programming that you do? And I'm curious about how that relates to what you're seeing from other state offices of rural health?
LISA: Our office was established here at Penn State in 1992. And we have been here at Penn State since then and have grown significantly. So, there's a state Office of Rural Health in every state in the nation. My office is one of 10 that are university-based. There are three that are 501C3s, and then the rest are in state departments of health. And so I think being at a university has been a great benefit for us because we have a lot more latitude in terms of the things that we do, although we work really closely with our state agencies, so health, human services, agriculture, economic development, aging, and so on.
And also [work] very closely with our legislature should they need any information from us, and so on. But really, where I think our sweet spot is, is knowing at an in-depth level what the issues and challenges, and successes are at the local, state, and national levels. Knowing what resources are out there, what the challenges are in accessing those resources, and in providing excellent technical assistance to those with whom we work and represent. So we may in fact be talking to a primary care clinic in a rural community, or we may be talking to a hospital that wants to convert a clinic to a rural health clinic. We might be working to bring about regional systems of care. We have a potential project like that up in the northwest where we have a pretty large maternity desert.
So we've been working with our partners to potentially implement a circuit rider program or make sure that the providers there are delivering very, very robust pre and postnatal care. Connecting that up with community health workers and having very clear plans for how a person, when they go into labor, can be transported for delivery. So you know, there are those kinds of processes that we do. We administer grant programs for very small rural hospitals. We work at just about every level in the state. And we also work nationally with all of our national partners.
So, there are a number of terrific rural health programs that are out there that either initiate or expand programs that are in states that focus on opioid use disorder, focus on rural maternity care. So it's a pretty broad spectrum of funding that's available.
SARAH: So here in Pennsylvania, you had started to mention this when speaking about the perinatal care and bringing folks together there, but looking at, you know, community health workers, community paramedicine, what are some of the other promising innovations you've seen here in the state?
LISA: When I came into rural health 30 some years ago, mobile health was a big trend at the time, and then it kind of fell off, you know, because it was expensive to operate and so on. It was 30 years ago and the equipment just was not as reliable. It wasn't as technological as it is now. So I think there are a couple of things that we are looking at in terms of where we can see some innovations. One is having communities invest locally in their healthcare delivery systems. Because healthcare is one of the top three employers in any county and in some counties it is the top employer.
So we want those dollars to stay locally. We also want to see a strong overlap between healthcare strategies and community and economic development strategies because one cannot exist without the other. You absolutely have to have a strong healthcare delivery system to bring in or retain a great economic community, and you have to have a strong economic community in order to be able to have a strong hospital. So they are intrinsically connected. We also are looking at the community health worker model, which I think is probably one of the greatest models that has started to flourish here in the state and across the country because community health workers come from the communities they serve. They understand the population. They understand what the issues are. They go through great training programs and they are supported by a healthcare delivery system. They can go out and intervene essentially and assess so that problems are addressed in the home or other ways rather than somebody coming to the emergency department. So I think that the community health worker model is just brilliant and I'm so glad that we now have the certification in the state for the CHWs. And I so hope that CHWs will be fully integrated into healthcare policy, payment and practice. So that's another way.
The other is to be looking at other kinds of services like doulas or by having mobile care, because I think that is now beginning to become very popular, not only with healthcare providers, but also in communities. Especially because we're 30-some years later, the equipment is pretty solid, and the vans are pretty solid. So being able to take that out into communities where Mrs. Jones knows that on every Thursday there will be someone in the parking lot of the Dollar General, let's say. She knows where she can go get some care.
The other is the state is investing a great deal through the Federal Infrastructure Act funds in high-speed internet because we have places in Pennsylvania where you just don't have any coverage at all and you also don't have very strong coverage. So if someone in your house is doing one thing with the internet, you might not be able to do another. So there was extremely good mapping that occurred by Penn State Extension to map the entire state to determine where it was well-served and where it was not well-served. And so I know there's been a focus through Pennsylvania Broadband Development Authority to get the funds out all across the state, but especially in those underserved areas.
SARAH: Historically, you know, rural health, telehealth, is the immediate connection and thought around access to care, How has that changed over the course of the pandemic, in recent years? Obviously, there's still a lot of work that needs to be done related to broadband. But what are some of the developments you've seen related to telehealth?
LISA: There have been several. When the pandemic started, there was suddenly this high demand for virtual care. And what was discovered, and I'll focus mostly on CMS right now, is that they were trying to reach a number of older patients who did not have access to high speed internet, did not have a computer, may not have even had a telephone that had any sort of a screen on it. So they were able to relax their restrictions on what qualified as a telehealth visit, because it had to be before, had to be with a provider where there was an already established relationship and it needed to be essentially video-to-video. So they relaxed that, which was terrific. And there was an enormous increase in the number of claims that Medicare received in just one month for telehealth services.
The other is that telehealth has become much more robust over time. There are a lot more procedures that can done via telehealth. You know, remote patient monitoring is one thing, you know, where you have a blood pressure cuff and so on and you're connected up and have a team monitoring. But other types of services are also so good now, where the diagnostics via telehealth are very sophisticated. You can listen to all sorts of body parts. You can actually do an oral assessment. We have seen telestroke for small rural hospitals that are connected up to tertiary care facilities so that there's immediate access to a stroke expert when someone is brought into the hospital.
We have a hospital here in the state, it's a Tele- ED, so that their emergency department is not staffed by emergency docs. It is staffed by physician assistants and nurse practitioners. If a patient should come in and they would need some assistance, they are automatically connected to a tertiary care facility where they are getting that service. The other big thing that happened in the state is that we were a state that did not have telehealth parity, meaning that there was no legislation that required all insurers to pay to reimburse for telehealth. And Senator Elder Vogel had tried several times to get something passed, and this last year, in this last session, he was finally able to get something passed, which is terrific. It does not set the amount for which telehealth needs to be reimbursed, but it does say that every insurance plan needs to reimburse for telehealth services.
SARAH: Thank you again for the just wealth of information that you've been able to share with us. Are there any final thoughts that you want to share before we wrap up?
LISA: I do want to say that rural matters. If you woke up this morning in a building that had wood, you had rural to thank. If you ate breakfast or lunch or a snack, you had rural to thank. And if you have clothes on that have any sort of natural fibers, you have rural to thank. And, you know, rural areas, especially here in Pennsylvania, you know, agriculture is our largest economy, as is tourism because of all of our state parks. So rural Pennsylvania and rural America contribute significantly to the overall economy and have benefits across both rural and urban areas.
So what I would like to suggest is that we never think about rural versus urban. There's really a continuum and they all need to be connected. And I would hope that if anyone is listening and they want to make sure that we have rural programming, at least for the next couple of years, that they consider how they might be an advocate for services in their communities.
SARAH: Well, thank you for your advocacy and work to keep rural Pennsylvania and rural America healthy. So thank you so much again for joining us.
LISA: Thank you. This was really fun and I appreciate the focus on rural.
SARAH: Special thanks to Lisa Davis for joining us. You can find our most current and past episodes of At the Core of Care, wherever you get your podcast, or panursingworkforce.org. For more information on upcoming webinars and trainings for nurses to obtain continuing education credits, log on to panursingworkforce.org on social media.
And on social media, you can stay up to date with us through our handles @nurseledcare and @panursingworkforce. At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder. I'm Sarah Hexem Hubbard of the Pennsylvania Nursing Workforce Coalition and the National Nurse-Led Care Consortium.
Thanks for joining us.
SARAH: This is At the Core of Care. A podcast where people share their stories about nurses and their creative efforts to better meet the health and health-care needs of patients, families, and communities.
I’m Sarah Hexem Hubbard with the Pennsylvania Nursing Workforce Coalition and the Executive Director of the National Nurse-Led Care Consortium.
On this episode, we're going to explore the current landscape of community health centers with PHMC Health's new medical director, Dr. Pheobe Askie. Pheobe supports PHMC Health's clinical staff across five community health centers in Philadelphia. She received her undergraduate degree in nursing and is now a board certified physician in both lifestyle medicine and family medicine.
Prior to coming to PHMC Health, Pheobe practiced family medicine in Louisiana.
Pheobe, welcome to At the Core of Care.
PHEOBE: Thanks, Sarah. I'm happy to be here.
SARAH: So we love hearing about how our guests got into health care. Can you tell us your story?
PHEOBE: If you ask my mother, she'll tell you I've wanted to be a doctor since I was two years old. And so how I actually ended up in nursing is the interesting story. I actually went to Penn's undergraduate visiting days and, you know, there was nobody at the nursing table. I was like, Oh, okay, I don't want to wait in line for the other things. So I'll just go talk to them.
And they told me all the wonderful things that Penn Nursing did and how great their program was. And I was like, Oh, okay, but I'm going to be a pre-med. And then the girl goes, Oh, I'm pre-med and the girl next to her goes, I'm pre-law.
And so they proceeded to kind of tell me about what the benefits of a nursing education was and, you know, as a 17-year-old, it sounded pretty convincing. I was like, Oh yeah, that makes sense. It's like such a great education. Why wouldn't I do that? I said, Oh, if I get into Penn, I'll be a nursing major.
And, good thing I did get into Penn. It was one of the best decisions I made as a 17-year-old. It definitely provided me with my passion, I would say. Because I was able to be more hands-on as a nursing student, I got to be in the community for the first time and actually worked as a community health organizer during undergrad.
And that is my lifelong passion now. I want to be where people are… I feel like there should be like an Ariel song. Somewhere in there.
SARAH: We won't start singing in this episode.
PHEOBE: No, nope. Nope. I'm saving you from that. And then so, even though I did go into nursing school, I worked as a nurse for a year because I was tired after exhausting four years, but then ended up eventually going into medicine.
I went to med school at Robert Wood Johnson and came back and, again, family medicine all the way at Jefferson. Ended up in Louisiana and got even more entrenched in community medicine there. Louisiana is such an interesting place. Such lovely people, but also so many health system issues that need to be addressed. And so I was really excited to kind of get my feet wet in community medicine there. I learned so much about how our healthcare system is helpful and unhelpful at the same time for people.
And so as I continue on my community health journey, I am very grateful to have been in Louisiana to learn where some of our opportunities are and some of our challenges in community medicine.
SARAH: So prior to recording this conversation, of course, you know got very excited about Pheobe's undergrad in nursing. But you talked about the relationship focus of nursing and how that's really stayed with you. Can you tell us a little bit more about that?
PHEOBE: Yes. I think that, whenever I tell people that I was a nurse first, I like, Oh, that makes sense. It's just a different model. In terms of the medical model where it's more focused on disease and nursing tends to be more relational. And, I think that's also probably why I ended up in family medicine and lifestyle medicine, because I feel like to be able to, treat people, you have to know them.
Like, I can't prescribe anything for you if I don't know what's going to work best for your lifestyle. So I feel like nursing taught me that. Not to say that medicine doesn't teach that now. I just think they're just a little bit later in the game. Now, I feel like the kids are going to be okay, they're selecting for kids who want to like have that relationship.
I feel as if, having your relationship with your primary care, clinician is so important, because you may be completely young and healthy at some point, but at some point, you're not going to be and you're going to need them.
SARAH: And so moving into medical school with that background in nursing, how did you see medical training as a nurse?
PHEOBE: I felt like I was better prepared than probably my peers were. I had already learned to work in teams and I knew who did what in teams. And I think that that kind of helped me in medical school.
It definitely made me more of an asset to the team I was kind of working with because I was like, oh, I know how that works. Let me just go ahead and do that. I suppose that it is something you learn in medical school, but it just kind of made me a little bit ahead of the game.
SARAH: And as a clinician, you've mainly delivered primary care, largely in community health centers. So, looking at things now, 2025, how do you define primary care?
PHEOBE: Wow. That is a big question. Primary care is very all-encompassing and nobody knows what we do. Everyone has a little bit of a separate definition. How I define it really is care to maintain health at the everyday level. It definitely is something that can encompass many different specialties, depending on where you are, and the skill of the person who you're working with.
How I kind of practice primary care is kind of kind of a journeyman sort of mentality. I try my best to just kind of meet people where they are, especially at the community health center level, like where people are. We'll go together. We'll do this health journey together. You'll ask your questions. I'll ask my questions. We'll come up with a plan. So I think of it more of as like a partnership.
And I think that's why primary care is so important. There's so much information out there, so much. The Internet will tell you you were dying. Do not believe the Internet. You might be dying, but talk to somebody about it. So I think that's why primary care is so hard to define because it's a lot of different things. But it is something that I feel like you do together with whoever's providing you primary care
SARAH: And something that's so nice about the community health center setting, and for those who don't know, community health centers, we're really talking about federally qualified health centers. We’ve had a couple episodes in the past looking at the health center program.
So when you're describing primary care, is that a certain population? Like, is that pediatrics or the whole family? Who are you serving in a primary care setting?
PHEOBE: As a family doc I really enjoy getting to know the mother, as she journeys, and then when the baby comes out, you get two patients, which is such a lovely thing to happen. And kind of watching people grow is something that I feel like a lot of people who end up in primary care really like and then, at the other end of it, is kind of journeying as people kind of get probably a little bit sicker, a little bit, less able to take care of themselves and working with the family to kind of make sure that they do that in a way that's dignified and gives people a really good quality of life.
SARAH: When I hear you describe family medicine, I really hear the family in it. So I always appreciate that.
So, zooming out a little bit, you spoke about, the health systems and the ways in which that maybe advances health and maybe doesn't in some cases. So looking at our current health system structure, we had talked a little bit about how insurance plays out and what it means for the continuity of care when your insurance may be changing and all of that.
So, curious about, you know, your perspective on that. So we're recording this in March 2025. What does that look like right now? And then we can think about what things might look like going forward.
PHEOBE: I feel like our current insurance system makes it really hard to have those primary care relationships that I think are really beneficial for people's overall health. I think a lot of times people's insurance is related to their jobs. And then if their job decides that they want to get a different insurer, that may change who they get care from.
And people don't really have a lot of say in that. On the other end of like non-profitized, insurance, like Medicaid, definitely has its benefits, but also has its limitations. I love it that people who are coming to our health centers get access to us, get access to care. I am worried in this current environment that Medicaid will not cover as many people as it currently is.
I think that being in Louisiana, I definitely heard horror stories before they expanded, Medicaid, that you would get a patient and then they would come to the ER and then you couldn't do anything for them. They would just basically keep on coming to the ER until something really, really bad happened to them because Medicaid wasn't expanded.
As opposed to post, like you didn't have as many options as private insurance, but you still had something you could offer people. And I feel like that is something I am worried in this current environment that we may have to face again. We might have to start making choices.
Especially during the pandemic, a lot of people where I was got access finally to Medicaid and like had a list of things that they actually wanted us to kind of handle. And it was just amazing to see people who never had access before get access and actually make some of those changes that was so vital to them feeling like they could be well again, like actually take the time during the pandemic to get healthier.
Which you don't generally think about during a pandemic, but people actually took the time to come see their doctors. I feel as if community health centers are a great space for, I always tell people, like, no, no, no, I don't care if you have insurance because that's the point of the community health center. Come see me. Oftentimes people will be like, well, I lost my Medicaid because I fell off the rolls for whatever reason.
And I'd be like - you know that I can see you without health insurance, right? You know that we do a sliding scale fee. And they're like, oh, I didn't know that. Because that's how non-community health centers, a lot of them work, is that they don't necessarily operate with a sliding scale fee, so they can't see uninsured for various reasons, which are very complicated.
But we at community health centers can. So I love that ability to see people regardless of their ability to pay or, even their immigration status. It's just something that I think that community health centers does such a good job at, and especially addressing some of the particular concerns in those communities.
SARAH: So, at the time of this recording, the United States Congress is working through a continuing resolution that was actually just recently passed. For those listening in the future, you'll know how this all turns out. The bill does include significant domestic spending cuts and, very much on the table, is the conversation about Medicaid.
So, right now, Medicaid provides health coverage to more than 70 million Americans, and certainly, all across the lifespan, including children.
You just described some of the ways in which, you know, just sort of being on Medicaid and being tapped into the Community Health Center Movement, you know, that you can kind of have that continuity of care, really focus on building that primary care relationship.
What would it look like for Medicaid to go away or to be scaled back in any kind of regard?
PHEOBE: Let's, you know, hope that with future listening of this, that does not happen. But if it does happen, that does put the operations of our community health centers as well as our rural hospitals at risk of not being able to stay open. Medicaid definitely provides that little bit of buffer so that we can be sustainable at our community health centers.
On the patient side, I think that it will look very dire. I hate to kind of be doom and gloom, but I do think that people will have a really hard time accessing the care that they need. And kind of will do what they did before, they'll wait until it's really extreme, until they're at the point where they can't not seek care. Which we know that that leads to worse outcomes.
So I really hope that we're not in the future time talking about Medicaid cuts, but that is something that I fear. I hope that people do kind of get tapped into community health centers because we can, somewhat, provide some care. We won't be able to provide the full gamut if Medicaid was to go away, but it is another access point to at least get some medical advice.
SARAH: Yeah. And for those less familiar with the community health center. program. So health centers, federally qualified health centers, do receive base funding from the federal government. It's not sufficient to operate, but it's certainly very important in developing those access points. And then certainly Medicaid for health centers as well as for hospitals, large health systems, small health systems, really do depend on Medicaid and Medicare for their operations.
So, certainly a lot of uncertainty, certainly something that we'll all be paying attention to, but that has a very real impact on individual lives as well as the health system as a whole.
So let's, focus on something maybe less doom and gloom, of maybe a little bit more positive and also cost saving actually. So talking about costs on one side to the other. The trend toward preventative medicine, what has that looked like in your time? Obviously you became board-certified in lifestyle medicine. Can you tell us a little bit about what that is? How did you decide to pursue that as a field? What does it look like?
PHEOBE: So lifestyle medicine is the prevention, treatment, and cure of chronic disease, through lifestyle modifications, We target six areas. We target obviously nutrition and diet because those are really important things. We really try to promote plant-based diets. Sleep, because, you know, if you, don't sleep, we all know the effects of not sleeping.
And then also good social connection, avoidance of risky substances like alcohol and smoking, and then, of course, mental health, making sure that is taken care of as well.
I got into lifestyle medicine because I was like, well duh. This makes sense. And really a lot of my patients were asking me things that they could do.
I feel like at the center of lifestyle medicine is autonomy. Like I am choosing to do these things that are helpful, but then also in there is the social determinants of health that we know that what I do as a clinician is very minuscule in the terms of like someone's overall health. And so I wanted to figure out a way that I could help people to help themselves essentially.
And I think a lot of people who kind of journeyed with me into lifestyle medicine felt like they were more empowered. They would come back to me and be like, Dr. Askie, I did this, this, this, and this. And I'm like, yes, go ahead. You're going to do this. You got this. And my job really is just to provide that information so that they know what they should be doing or shouldn't be doing.
Change is not easy. So my support is like to kind of just help with people who struggled with that change. So I felt like lifestyle medicine was a great way to practice primary care. Cause I was already telling people how to do things, but, you know, your doctor tells you to go eat vegetables.
Great. Okay. What am I supposed to do with that information? Of course I know I'm supposed to be eating vegetables. Of course I know I'm supposed to not be smoking, but how to make that actionable is why I went and got that extra board certification in lifestyle medicine.
SARAH: And now you're back in Philadelphia overseeing five community health centers. And also for those not in the area, PHMC Health is responsible for the nursing services in the shelter system in Philadelphia and operates two medical respites. So it's a rather large portfolio, lots of different kinds of lifestyles, lots of kinds of healthcare being delivered.
What are you bringing to this new role from your work in lifestyle medicine, your time in Louisiana? What are your hopes and dreams?
PHEOBE: Oh, I have so many hopes and dreams. I really, really love the mission of PHMC. I was like, man, they provide a medical respite. How awesome is that? Like, it just makes sense. Somebody's sick. They should not be going back out into the street. They should be having a place where they can actually rest.
And then they're where people are in the shelters. Like, I really, really loved the mission of PHMC. What I hope to bring to PHMC is more of the lifestyle pieces of it. Trying to incorporate more community engagement so that our health centers function more as a medical home, a place where people really feel connected to their community and their health care team.
We are doing a lot of new things. We just recently added podiatry services, so that's super exciting. Then we're trying to expand our mental health program and including child psych. We're also trying to expand in general pediatric services.
So I am really hoping that we can become even more entrenched in the Philadelphia community, which we are. I really want that to grow. And I really want us to be a space where we are helping communities grow healthier every day.
SARAH: Well, and I know for us and for those who have been listening for a while, you know, that at NNCC, we do a lot of maternal child family health and really are excited that, that Dr. Askie will be able to bring some of that expertise to care for newborns, to care for mom, to care for family. So definitely excited about that.
PHEOBE: I'm also excited about that because we are also working to expand our reproductive health services as well. I was like, I say in my former life, but I was a reproductive health advocate, but you know, I'm still that and so I'm hoping that we can offer more family planning services as well as support anybody who wants to be pregnant, to maintain a healthy pregnancy, and then to also have a healthy childhood for those Children.
And we're going to work with NNCC and the Nurse-Family Partnership to continue connecting our patients to their community.
SARAH: And I know that for those who are very familiar with federally qualified health centers, you know that things like behavioral health, dental, podiatry, are really all seen as part of the standard of care. But for those who aren't, you might be surprised to hear about some of those services.
Can you just share a little bit about behavioral health consultants and what that kind of holistic model of care that we typically see in a community health center?
PHEOBE: Another reason why I fell in love with community health centers a long time ago is that they really do try to do one-stop shopping. So, you can come see your primary care clinician and then, on that same day, you're like, you know what, I really want to talk about something that's going on. Maybe it's surrounding your diabetes and you want someone to kind of work with you in terms of, like, the emotional side of diabetes, which there is. It's not just a physical problem.
We have our behavioral health consultants. They'll see you that same day and then, if you need to feel like there's more depression or anxiety kind of going on around that, we will do a nice little warm handoff and you can meet one of our psychiatric providers.
And, if you're at the right clinic on the right day, you might be able to even walk in for dental services. So that model of where we can have seen multiple different people in one day and one day off from work because I, you know, you are taking time off from work. So if you're going to take time off, might as well get it all done, is something that I really love about community health centers.
And we at PHMC definitely do that as well.
SARAH: I think that there's so much about lifestyle medicine, about meeting people where they are, that we do need to make it a little bit easier to maintain health as you had kind of set us up from the beginning.
So, coming full circle to nursing, to relationships, Why do relationships matter in health care?
PHEOBE: I think relationships matter in healthcare because we don't actually know when things are going to go awry, but they do. And having that relationship when you're well can really make it much easier to access care, and to have somebody actually know you and what your goals are and what you wish for, and that time of need. That just takes away so much stress when you're like, ahh I'm in the middle of these strangers and they don't know me. They don't know why I didn't come in for this until now. They don't know anything about what's important to me, what my goals are.
So really that relationship helps people care for you, and I know we all know that going into urgent care, they don't really know you, they're just trying to solve a problem and you kind of feel like I'm just a number. But when you get that personal relationship that you have with your clinician, who knows you and knows your wishes and desires, I feel like it creates a better outcome. And you're more able to kind of manage when you really, really need help and support.
SARAH: We're coming to a close in our conversation today. Do you have any final thoughts you want to share with our listeners?
PHEOBE: Call your Congress people and tell them to support funding for community health center. I really do think that community health centers serve a special place in communities across the country, not just here in Philadelphia. They provide care to people who wouldn't otherwise get care, but then are also a great access point for anybody who needs care.
SARAH: Well, you have your instructions. Pheobe, thank you so much for making time today. It's been a pleasure having you. We'd love to have you back sometime.
PHEOBE: Thank you. It was great talking to you today, Sarah.
SARAH: Special thanks to Dr. Pheobe Askie for joining us. You can find our most current and past episodes of At the Core of Care wherever you get your podcasts or at panursingworkforce. org. For more information on upcoming webinars and trainings for nurses to obtain continuing education credits, log on to panursingworkforce.org.
And on social media, you can stay up to date with us through our handles @nurseledcare and @panursingworkforce. At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder. I'm Sarah Hexem Hubbard of the Pennsylvania Nursing Workforce Coalition and the National Nurse-Led Care Consortium.
Thanks for joining us.
SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families, and communities. I'm Sarah Hexem Hubbard with the Pennsylvania Nursing Workforce Coalition and the Executive Director of the National Nurse-Led Care Consortium.
On this episode, we're going to have a conversation about the latest trends in primary care with Chanel Hart. Chanel is the Director of Nursing for PHMC Health in Philadelphia, where she oversees clinical nursing care at the organization's community health centers and shelter and respite services for people experiencing homelessness.
As a registered nurse, Chanel worked previously across various hospital settings and taught community health nursing. Recently, she earned an MBA and serves as the board chair for the National Nurse-Led Care Consortium, as well as the Vice President of the Philadelphia chapter for the Chi Eta Phi sorority, which is the first black nursing sorority in the United States.
And finally, Chanel is a board member of the Nursing Foundation of Pennsylvania, as well as a member of the American Academy of Ambulatory Care Nurses and the American College of Healthcare Executives. Chanel, welcome to At the Core of Care.
CHANEL: Thank you so much for having me.
SARAH: Chanel, you're among some of the most passionate nurses I know, and I know a lot of very passionate nurses.
But I actually did not know that nursing is your second career. I'd love to hear the story. How did you decide to become a nurse?
CHANEL: Okay, well, I've always worked in nonprofit. My very first job out of high school was working for Elizabeth Blackwell Health Center for Women. From there I went to the Youth Empowerment Services. So, within Youth Empowerment Services, we applied for a grant from the Beacon Schools, in New York.
So this was a 3 million grant to bring programming, after-school, and summertime programs to the children in some of the communities throughout the city of Philadelphia. So my grant was actually for Sayre Middle School.
So I thought if I ever left nonprofit, I would go into nursing. After I left, I went to EMS school at Jefferson and became an EMT to see if I even liked patient care. And from there, I went on to become a nurse. My manager at the time, who is no longer with us, pushed for me to apply to Dixon School of Nursing.
And I think she was more excited about me getting in than I was.
SARAH: And here you are today. So joining us at PHMC in 2022 as the Director of Nursing. And at that time, COVID-19 was very present in all of our lives and certainly through the clinical care here at PHMC.
CHANEL: So before I came to PHMC, I was at Jefferson Family and Community Medicine. So, we were kind of like in the heart of what was going on as far as COVID goes, because I facilitated a site on Jefferson's campus for people to come in to get vaccinated. At the time, they were calling the nurses back into the hospital. So if you left critical care, you had to go back in.
I did two, three weeks in the neuro ICU. So it was definitely a time. It was like being truly in a battlefield, at that point. And I remember the doctors, I remember the residents being afraid to address these issues. And who was it? Of course, it's us, the nurses leading the charge.
I remember a time I had two attending doctors and a student and they didn't want to go in to speak to an elderly patient that came in with respiratory symptoms. And I was so frustrated by the whole thing. I just kind of like put my mask on and went in the room and spoke to the patient.
And as I'm talking to her, I asked her which one of your grandchildren has the runny nose and she started laughing and said, Oh, two of them. I had to babysit while they were sick and she did not have COVID. Thank goodness. She had a basic cold from two of her grandchildren that are in daycare. But that kind of set the tone, I think, bringing nurses back up to the forefront.
And I was very glad to be a part of that. And seeing all of it just gave me a whole different outlook on the role of nursing and ambulatory medicine.
The outlook for nurses in the ambulatory care setting is definitely changing and the idea of them working at the top of their licensure is going to be vital.
SARAH: So now that you've been here at PHMC, I know that you've been part of a lot of different initiatives that have rolled out. One of the more successful initiatives, and certainly, on the radar, even nationally, you know, looking at, how we are engaging patients through digital tools, you helped design a blood pressure initiative, right? Can you tell us about how that project worked and the role of nurses how that rolled out and what success looked like?
CHANEL: When I came on board, the American Heart Association had a blood pressure program that they were initially just starting. But the person that was here before me was the one that took the charge. And once they left, I kind of picked up to see where we needed to work with this program. So the grant was in partnership with Bank of America for a $25,000 grant that we got to improve blood pressure with some of our patients.
So working very closely with the American Heart Association, utilizing tools that I found off their website, I was able to create an algorithm that allowed the nurses to lead the charge in reference to new patients diagnosed with hypertension.
So, essentially the patient comes in, they're diagnosed with hypertension. That generally takes three office visits. No one's ever, the very first time, oh, you have high blood pressure. Go be on medicine. But once the patient is officially diagnosed, the providers give a warm handoff to the nurses to let them know. Once the nurse gets involved, we can now schedule more visits with the patient versus them seeing the provider.
So the tool has everything from identifying the blood pressure, the social determinants of health, going over medication reconciliation, understanding where we're trying to get the patient to. And utilizing the monies that we got from the American Heart Association, we purchased Bluetooth-compatible blood pressure cuffs so that the patient can actually hook it up to their phone.
Of course, theres challenges when you have populations that are unhoused and at any time their phone numbers can change. So they have a paper tool that they can log in. Then they come to see the nurse. It could be every two weeks until we get the blood pressure where it needs to be. Once that happens, then we see them monthly and we record their success. A copy of the algorithm is put into the Epic system, that’s our EMRS system, to allow for us, when we're documenting, where we're reporting the metrics, that we can actually go right into EPIC and pull the numbers that we need. Because it is identified as self-measuring blood pressure RN note, so that, you know, it's easy to find. That's the most important part with documentation and data, making it easy to find.
We've been very successful and I'm very proud of the nurses at the sites where they reach silver status with the American Heart Association. So it comes in three tiers, of course, bronze, silver, and gold. So reaching that milestone of silver, especially on our first try at that, I'm very proud of them
SARAH: What did you hear from patients who participated in the program? What did the patients have to say?
CHANEL: The feedback that I got from the nurses is that the patients appreciate having access to care. And that's how they looked at it, having access. If there were questions about why their blood pressure kept rising that they could not fix, then they had someone that they could go to and it didn't necessarily have to be their doctor.
The patients do come back and that's the most important part. That becomes a huge bottleneck in trying to add any of these systems into place is getting the patient to actually come back to the office. So our no show rate actually is reduced when the patient is coming in to see the nurse versus the provider.
SARAH: Do you have additional thoughts on why folks are coming back to check with their nurse? Like what do you think's behind that?
CHANEL: I would like to wear this banner that say, cause nurses are just so amazing. But, realistically, I think that it is the amount of time that the nurse can actually give to the patient and the patient does not feel rushed. One thought that I've gotten from patients is they feel heard.
So even if I'm at the site and there's an issue or a discrepancy, when I intervene and introduce myself as the Director of Nursing, they are telling every single thing that they could possibly think. They appreciate their MAs, they appreciate their nurses. They speak highly of the nurses. Because the biggest part is that it's the time allotted for listening.
So we just have to take those couple of extra minutes to actively listen to what our patients are saying to make them feel valued and heard. They feel like talking to nurses is a safe space and they tell everything.
SARAH: And so that's really just one example of the role nurses can play in primary care. And there's been a lot of attention to this, of really looking at the role of the of the registered nurse. I know you've certainly given us a lot of thought around transition of care and other models. You know, tell us a little bit about the transition of care and how we are supporting patients when they are discharged from the hospital.
CHANEL: Of course, this was my MBA final project. But, this is very close to my heart because we're missing out on great opportunities. The evidence shows that patients are their most vulnerable from discharge to going home. So trying to figure out a way that we can get the patients in in those allotted times and it's generally 7 to 14 days post inpatient discharge.
And it's important to understand the difference. Just because they went to the ER, it doesn't necessarily fall under that 7 to 14-day window that they need to see their primary care. But if they have been inpatient, then you have to see them according to the insurance companies to stay in compliance with that transition of care metric.
One thing that I found doing the research is our providers are just busy. So, the best way to utilize this is using our licensed nurses to kind of lead that charge. When you look at what is identified as a transition of care appointment, it is really basic, discharge review, medication adherence, making sure that patients have the referrals they need, should they need to go follow up with a specialist, making sure that they have DME, which is their dural medical equipment, at home.
So, if this is all you're going through, you might do wound checks. The nurses can start that and they can also see the patient a little longer than a 15-minute slot. So they can actually have a 45-minute appointment to get to basically the meat of everything that's going on. And then a 5 to 10-minute follow-up with their primary care to be able to bill for that service.
So this gets the patients in faster, it allows for a more comprehensive overview of why they were in the hospital, helps to support follow-up, and creates a level of trust between the families and the patients and the healthcare provider. Plus it can close that bridge gap between the health care center and the hospital because now the hospital's care managers know exactly who to call.
We know the back story and then we can go head-on through to make sure that the patient has the best possible outcome. Because at the end of the day, that's what's important. To make sure that they did not have to return to the hospital within that 30 day window, which is cheaper for the health system, it's cheaper for the insurance company, and it gives the patient the best possible outcome.
SARAH: So there's really a lot of value to having the nurse manage really most of that transition of care visit. What are the implications in terms of billing? I mean, how, are health centers reimbursed for nurse visits?
What does that look like? I know that, you know, in the acute care setting, this is often a topic because nursing care is included in the bed rate. And so the actual nursing service is often lost, right? We don't see that reflected in billing. What does that look like in the community health center setting?
CHANEL: Unfortunately, nurses' time is not billable in reference to office visits. So, if it was a nurse that was going to the home, doing home care or doing patient wound care. That's billable time. Last year, they made it CHW's community health workers' time billable, yet nurse's second most expensive cost in clinics is still not billable, yet we can do so many things.
It would be ideal. The conversation is actually on the table with the Pennsylvania Board of Nursing, but it has not trickled down. When you look at the expense of having a nurse and I don't mean in dollars and cents, I mean in value as far as experience, education, the time for patient care. It's invaluable, but there is value added to it and we should be able to bill for that.
That will also make our clinics stronger. Yes, the provider can bill for it, but the nurses adding so much value to it that somewhere we should be able to bill for the nurses' time. That way, maybe more primary offices will take on nurses to support that. You know, medical assistants fall under the licensure of the provider, whereas nurses, we’re our own license and we must have a license to practice in the state of Pennsylvania.
So, if we have to have that license anyway, we should be able to bill for the time that we are spending with those patients. So, insurance companies should really take a deep dive, and see how being able to bill for ambulatory care, we bill for health coaches. The insurance companies definitely can get paid for their nurses to be health coaches.
We are essentially health coaches in the primary ambulatory office, and we should be able to bill for that time.
SARAH: Yeah, definitely seems like things align there to the benefit, again of reducing cost, and achieving the goal of that transition of care appointment. So this is an area to watch and an area of opportunity.
So, from a broader professional development viewpoint, what are some of the clinical trends that you're seeing, related to utilizing registered nurses in primary care, but also related to training, to preparing registered nurses to practice in primary care?
CHANEL: Working in primary care is not taught in the classroom, yet it is something that is greatly needed. When I came to PHMC, understanding that they were going to have nurses that we interviewed that had never worked in primary care, I created a book for the ambulatory care nurse to understand the transition of going from inpatient setting to primary care.
It explains their scope of work, which is very important. So you understand that your scope of work in primary care is very different than when you're working bedside, meaning there's a huge level of autonomy for nurses that work in primary care.
And there is a level of respect that comes from understanding vaccines for the children, understanding gerontology, and knowing how to do a DME and a prior authorization. These are things that at the bedside, you know nothing about. So when you come into this environment, this is where you learn how to navigate working with the insurance companies, how you navigate working with the city of Philadelphia, because if you do anything wrong with vaccines and vaccines for children that could shut down your entire program.
Ambulatory medicine is Monday through Friday, 9 to 5. No nights, no weekends, no holidays. So, it definitely has its perks. It would be exciting if we had the opportunity for more schools to get into showing their students what it's like to work in primary care.
Currently, I am working with Independence Blue Cross to have nurses come in during the summer to do their summer internship. One of the requirements that I asked for is for them to write an essay on why they would be interested in public health.
Public health is so important to our communities and the joy of having a nurse in each center. Some of our sites, we have two nurses. It's unheard of.
SARAH: And I mean, you just spoke about this directly, but really looking to the next generation of nurses. How, can we cultivate a pipeline of nurses that can be those registered nurses in primary care, that, growing workforce? Where are opportunities?
CHANEL: Funny you should ask. I had a meeting this morning with a charter school in Center City who would like to bring some students to shadow nurses for eight weeks. And they receive a stipend from the school for eight weeks for 3 hours a day, they get to shadow our nurses and the students who are selected for this program are interested in nursing. Getting them touched by nurses now is going to be vital. Because what we're finding is high school students are struggling still with math and science.
And nursing is essentially an extension of STEM. So this is an opportunity to get our Philadelphia schools into STEM programs at the high school level. The good thing is when they come this summer, I'll also have nursing students. So getting them in touch with nursing students who are actually going through the process of nursing school, and then they're working with nurses who are doing the job and leading the charge.
Reaching them younger, I think, will benefit us in the long run. Because when you get them at the college level, what they're hearing the most is you have to go in to be a nurse practitioner. When I taught, most of our students wanted to be nurse practitioners, but we're losing all the other nurses.
We're losing ambulatory nurses, we're losing bedside nurses, because it's the glory of being a nurse practitioner. We have to get back to, don't forget about the basics. We need our nurses. We need them in the schools. We need them at ambulatory centers. We need them in surgery centers. We need them out in the community.
SARAH: You captured so many important themes here and we often talk about having all professionals practicing at the top of their license. And that's very much true of the registered nurse, that a registered nurse is able to do so much and is often not being fully utilized in a practice setting, whether that's in primary care, frankly, or by the bedside.
So I think there are a lot of folks really paying attention to this and how do we maximize every professional in the care team and get to those quality outcomes, improve the patient experience, reduce costs, right? All of the things that we've been talking about. And the role of the registered nurse comes up again and again in those conversations.
I did want to add a plug when you mentioned nursing and the relationship to the STEM disciplines. So science, technology, engineering, medicine. There is a movement, and I wanted to call out to amplify nursing out of Penn nursing, Marion Leary and another colleague, Rebecca Love.
They have been great leading a coalition to get nursing recognized as a STEM discipline and see the benefit to that designation because you're right, these are the skills that are needed for nursing and that we want to prepare that pipeline and get those benefits.
So we're coming to the end of our show today. Any final thoughts do you want to share with our listeners?
CHANEL: Looking at nursing from where I started to where we are right now, I have had just some amazing opportunities. When I first had the, where do you see yourself in five years? This was not it. I thought I would still be at the bedside. I still thought that I would be, with my patients and I do miss them.
But given the opportunity to help nurses reach their fullest potential. Being able to mentor, I mentor nurses at Widener University and at CCP. I volunteer to help them understand, their nursing concepts to be a role model for people I don't even know. And then looking my daughter decided she was going to go back to school for nursing. And when she went she's giving these people my resume, and I said, well, you know, they were asking you about you and she said, well I needed to tell them all the wonderful things about you. You never know who you're touching, and nursing touches so many people, that you only need one to really feel like you've made a difference in the world.
So I am very happy with the choice that I made to be here. I hope that I am moving in purpose on purpose, and I hope that it inspires a new generation of nurses and nurse leaders to continue to lead that charge.
SARAH: Chanel, thank you so much for what you do every day at PHMC Health, what you do for the nursing workforce, what you do for us at NNCC. Just really appreciate your commitment and thanks for making time for At the Core of Care.
CHANEL: Thank you for having me. I've really enjoyed it.
SARAH: Special thanks to Chanel Hart for joining us. You can find our most current and past episodes of At the Core of Care, wherever you get your podcasts or at panursingworkforce.org. And if you're interested in learning more about the role of the registered nurse in primary care, check out our resource library at nurseledcare.org.
For more information about upcoming webinars and opportunities to obtain Nursing Continuing Education credits, log on to nurseledcare.org. On social media, you can stay up to date with us through our handles, @NurseLedCare and @PANursingWorkforce. At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder.
I'm Sarah Hexem Hubbard of the Pennsylvania Nursing Workforce Coalition and the National Nurse-Led Care Consortium. Thanks for joining us.

We are filled with so much gratitude as we enter the holiday season. Thank you for your endless dedication to your communities and to the nursing profession. Thank you for joining us throughout the year to develop creative solutions to advance healthcare in our state. Thank you for sharing your insight and expertise on our committees, webinars, and in-person events.
We look forward to an exciting 2025 as we embrace our new chapter as the Pennsylvania Nursing Workforce Coalition and expand our partnerships and programs. We hope you and yours have a happy, safe, and peaceful holiday season and we will connect with you in the new year.

SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families and communities. I'm Sarah Hexem Hubbard with the Pennsylvania Nursing Workforce Coalition, and I'm the executive director of the National Nurse-Led Care Consortium.
One of our core strategic goals at the Pennsylvania Nursing Workforce Coalition is to support the next generation of nurses. It's part of our efforts to bolster nursing workforce pathways. Since 2016, as part of our Pennsylvania Nurse Residency Collaborative, we've partnered with Vizient Incorporated to implement nurse residency programs at more than 70 hospitals across Pennsylvania, and to help new nurses make the transition to becoming professional registered nurses.
On this episode, we're going to talk with Deborah Gardiner about how the Nurse Residency Collaborative works. Deb lives and breathes nurse residency programs. As one of the co-chairs for the Workforce Coalition's Nurse Residency Collaborative, she shares her expertise from her day job as the Nurse Residency Coordinator at Thomas Jefferson University Hospital in Philadelphia.
Deb is also a Nursing Professional Development Specialist and Nurse Leader for the hospital's RISE program, which is part of a nationwide initiative to support healthcare workers coping with stressful or traumatic patient-based experiences. Deb, welcome to At the Core of Care.
DEBORAH: Sarah, thank you so much for having me here. It's my honor and privilege to speak on a profession that is so near and dear to my heart.
SARAH: So, Deb, we love hearing about how our guests got into nursing. Can you share your story with us?
DEBORAH: Yes, so I do come from a long line of nurses. My great-aunt was an army nurse. My aunt was also a nurse. She got her doctorate in nursing, and she taught in the nursing profession.
In the undergraduate program, and I've always heard about so many wonderful and romantic stories and heroic stories of how my peers and my colleagues got into nursing. But my story is a little bit different. I was in high school. I was a junior and I was asked to participate in a blood drive. At my high school and I had the opportunity to take individuals after they donated blood to walk them to a refreshment station to get orange juice and cookies and I got home that night and I said, I want to be a nurse.
So maybe again, you know, hearing stories of maybe someone struggled with an illness in their life and they had been touched by wonderful nurses and that's why they wanted to be a nurse or they had family members in the hospital and that's why they wanted to be a nurse. I always thought that my story was insignificant in comparison to theirs, but what I have learned over the years. Um, to understand and appreciate is just the core of my story, which comes from that basic element of caring. And that is what really binds us all as nurses together. We have that common bond of caring for another individual and making them feel better.
SARAH: I love that. That's beautifully stated. So, you made the transition from working clinically in surgery and trauma to becoming a nursing professional development specialist and now, of course, the nurse residency program coordinator. So, tell us a little bit about how you made that transition and what excited you about it.
DEBORAH: So, you know, I started nursing in 1990 as a brand new GN during a time when there was a nursing shortage. So, I was very fortunate to have the opportunity to choose from many hospitals within the Philadelphia area. And I did choose Jefferson Health. It gave me a wonderful feel. The people were warm and exciting, and it felt like an extension of my family. So, I've been working at Jefferson for 34 years now in surgery and trauma.
I spent about 15 years of that time as a clinical nurse specialist. So, mentoring new to-practice nurses as they started out their journey at Jefferson in surgery and trauma. So, then I thought maybe it's time to challenge myself to allow myself to learn and grow. So, I transitioned about three years ago, became a nursing professional development at Thomas Jefferson University Hospitals, Inc., and coordinated orientation for a little while. And then the opportunity arose to be the nurse residency coordinator. And this was a program that I felt deeply committed to and really found such value in meeting and supporting those new to-practice nurses. And it was a program that I had taught in for many years.
So, I started in 2009 teaching in the nurse residency program at that time as a clinical nurse specialist and taught the curriculum of changing patient conditions, chest tubes, bullying delegations, and then clinical reflections or tales from the bedside. So, it was just a huge honor of mine and maybe a dream at one time to be the nurse residency coordinator because again, it's a program that I'm deeply passionate about and committed to.
SARAH: So curious when you started as a nurse, did you go through a residency program?
DEBORAH: So, when I started we didn't have the nurse residency program, but we did have resources at that time you had a unit-based preceptor to help support and guide you and mentor you, and then we had unit-based mentors And we had a clinical specialist based on each of the units. So, um, we did have systems in place at that time, but it certainly wasn't, um, the nurse residency program.
SARAH: So, fortunately for us, right, you, um, joined our Pennsylvania Nurse Residency Collaborative Steering Committee in 2022, and became a co-chair in 2023, you can tell from our interviewee that, um, we've got a go-getter on our hands. So, let's talk about what new nurses can expect when they go through the Vizient Nurse Residency program here in Pennsylvania. What are the three key areas of this evidence-based curriculum?
DEBORAH: The Vizient Nurse Residency Program is a wonderful program that assists in the transition of that new to-practice nurse from that advanced beginner to the competent nursing professional. So, the residency program started in 2002 as a multi-state research study based on the need to say, we have large volumes of new-to-practice nurses starting out. What do we need? What systems do we need to put in place to make sure they feel supported and to make sure that they are retained within our health care organizations. So, the nurse residency program is just an added layer of support for our new-to-practice nurses when they first start out beyond their orientation and beyond their precepted experiences. And the Nurse Residency Program is a 12-month program. So as coordinators, we meet with those nurse residents over the course of their entire first year in practice in order to support them as they transition. So, some of our other goals of our Vizient at Nurse Residency Program is to help them develop effective decision-making skills and clinical judgment skills for those new-to-practice nurses so that they can practice safely in the healthcare environment. We also provide them with clinical leadership skills.
We support them and promote their development in interacting with that interprofessional healthcare team. We like to strengthen their commitment to their chosen profession of nursing. We also help them get engaged in their healthcare organization and within the hospital. And then we incorporate an evidence-based practice project within that program.
So, there are many different domains that we teach to. We have many different curriculum elements. We look at their development as a professional nurse. We look at the foundations of quality and safety within the nursing profession. We look at their interprofessional practice. their knowledge for nursing leadership and system-based practice, and we focus on person-centered care. So, there are many different elements. And then we do look at the scholarly aspects of nursing care, such as the evidence-based practice project that I mentioned about a little bit ago.
SARAH: Thank you so much for providing an overview of the program. And, you know, we've definitely been able to see firsthand, you know, the impact of the program as well as how it rolls out in sort of nuanced ways, depending on the institution and, you know, throughout the state. So, on that note, we're going to hear a brief clip now from Bianca Innaurato, who, like you, Deb, is a nursing residency coordinator and nursing professional development specialist, but at the University of Pennsylvania.
BIANCA: I think what gives me hope about the future of the nursing workforce is seeing the nurse residents come into the hospital month after month with the same excitement and hope for their careers that the previous cohort had.
So, I think it's nice that. People are still excited to come in. They're really passionate about their career. They're so eager to get started and they're really listening and hanging on to every word we say in nurse residency, especially in those first couple of seminars. So, I think that's really the most exciting thing for me and working with the nurse residency team at Penn Medicine is one of my most favorite things because we are really a close-knit team and everybody is really fun and upbeat and we all feed off each other and kind of energize the crowd.
SARAH: So what we know from the collaborative is that nursing residencies are supporting nurses who are, you know, developing their skill set, the specific knowledge around safe and high-quality care, also sort of supporting them in that to take it to the next level, looking at leadership and professional development in the ways that we know also support recruitment and retention. So, most states across the country, with the exception of just a few, do have some kind of residency program. What has been the buy-in piece? So why are health systems, why are hospitals engaging in this type of curriculum and looking to nurse residency programs?
DEBORAH: The reason why there's such a strong buy-in from our healthcare organizations is what we have found is that those hospitals that engage in nurse residency programs have new-to-practice nurses that have higher retention rates. There are lower turnover rates in those hospitals, and those new-to-practice nurses are more satisfied in their jobs, and we retain them within the organization, which is really so important because when you think about the average cost, To hire a new employee and go through orientation.
We're looking at some figures from 68 to 88, 000 dollars per nurse. So, when you think about the return of investment, we are investing a lot of time and money, and energy orienting these nurses. And we want to retain them at our organization. And what we find is those healthcare organizations who have those nurse residency programs, are retaining the nurses at the bedside.
SARAH: So, help walk us through the nurse residency program that you oversee. How does it work? Are new nurses automatically enrolled? How long do they stay with the program? Sort of, the operations, logistics, how does it work?
DEBORAH: So, we work very closely here at Thomas Jefferson University Hospitals, Inc. Um, to work with our HR department.
So, every time a new group of nurses starts an orientation, it's reflected on an HR spreadsheet that they are a new-to-practice nurse. So, they are automatically, as a provision of their employment here at Jefferson, automatically enrolled in the Nurse Residency Program. I meet with them on their first day of orientation and explain the Nurse Residency Program and why it is so important. I give them a schedule for the entire year of our nurse residency program. We meet about every six weeks with our nurse residents over that course of the year. And the way our seminar is structured is that we have definite elements that are incorporated within each of our nurse residency seminars. So, we have a welcome to the group.
We also break out into small group sessions. They are called clinical reflective sessions. So, we take that larger group of nurse residents, we break them up into a smaller group, and we discuss a clinical topic. Tell us a time when you had a changing patient condition. Tell us a time when you had a very challenging patient. Tell us a time if you had a patient get some upsetting news. So, it is an opportunity that allows them to openly reflect upon their practice so that they can learn and grow. We also have a segment in our nurse residency every time we meet with them called Reflective Rating Exercises. Again, another opportunity for them to learn and grow as they reflect upon their practice.
We always break out into EBP lab where we will work on an evidence-based practice project. We always incorporate some piece of mindful breathing exercises as a way for them to learn how they can take care of themselves while they are taking care of their patients. What can they do to help themselves and support their own well-being? And then scattered then throughout the rest of the day are elements of our curriculum based on the domain set forth by our Vizient curriculum.
SARAH: And you had mentioned before the evidence-based research project. So, can you share a little bit more about that?
DEBORAH: For all of our nurses, we really do encourage that spirit of clinical inquiry.
So, examining your practice. Why are you doing what you're doing every day as a nurse? is this best practice and what can we be doing better? So, we incorporate an evidence-based practice project. It is one of our goals through Vizient. So, we start off in Seminar 1 when we meet with the residents and they form small groups with other nurses that are working in a similar unit as them.
And then each seminar beyond that, builds upon the elements of the evidence-based practice project. So, the goal of the evidence-based practice is for them to be able to examine their practice and to understand the steps of engaging in that evidence-based practice. So, after they leave residency, if they identify an area for opportunity on their unit, they already know what they need to do when they are examining their practice.
So then in Seminar 2, they pick a problem. What is an opportunity on their unit that they want to explore to see if it's best practice? They develop a PICO question. In Seminar 3, they perform a literature review. In Seminar 4, we look to the literature again in Seminar 5 and say, what did we find in our literature to support a best practice? And then in 6, we implement, and we evaluate our outcomes. And Seminar 7, which is our final seminar in residency, the nurse residents stand up and they present that EBP project to their peer group. To that cohort group and to the leaders of our organization and what I tell the residents is that although we are here from them that this may be one of their least favorite parts of nurse residency. When we had our nurse residency accreditation survey in the fall of 2023, the surveyors who met with some of my current and former residents, they said, you may never hear this on any report from our evaluation of your program, and you may not even hear this from your residents, but after speaking to those former residents and present residents about their EBP project.
They did identify it was probably their least favorite part of residency as they were going through it, but they did say that they found such value and meeting at the end when they were able to stand up and present their project to their peers. So really, again, in residency to touch a life is to change a life. And, you know, that is so rewarding and gratifying. To me, to help them through this process.
SARAH: And I think that we, we hear that from nurses, right? So, the way that you're speaking about residents really have that parallel process to nurses caring for others. So, we know, you know, there's no nurse who's the same.
Nurses, like many other professions, represent a diverse group of individuals and backgrounds. The same is absolutely true of, um, patients and the communities they serve. One of our nursing collaborative steering committee members, Brianna Blackburn, she's an instructor of nursing and a PhD candidate at Penn State University. She sent us her thoughts on what she's seeing in this latest generation of nurses ready to enter the workforce.
BRIANNA: I am a registered nurse and an educator in the state of Pennsylvania, and I think we have so much hope and things to look forward to. For the future of nursing in my students, I see a new level of commitment to understanding and respecting the diversity of the patients in which we serve and a commitment to creating a nursing workforce that accurately represents the communities in which we provide care.
I also know that our students are more focused on mental wellness, both for themselves and for our patients, much more than those generations that have come before us. Given that this is a national issue and something that has long gone underserved, I look forward to seeing what the latest generation of nurses can do to help us progress in this area.
SARAH: So, Deb, after hearing from Brianna just now, um, you know, broadly speaking, and especially thinking about the hopefully post-pandemic healthcare space, how can we build up and sustain strong support systems for nurses over time?
DEBORAH: So, again, something that is very, very near and dear to my heart is how do we support our healthcare providers on so many levels, not only our nurse residents but the nursing profession as a whole.
And I am so thrilled to say now more than ever, we've seen this shift to the well-being and the holistic health of our healthcare providers. So, for us at Jefferson Health, we have so many. Programs available to support our health care workers across the organization, whether they are nurse residents or are nurses or any of our providers across our hospital. So, we have some of our self-help resources that are available to our nurses. There are online apps, there are, um, something called a Marvin app where they can go and they can get some mindful breathing techniques. We also have an additional level of support. We have the Rise program. So, I am the co-chair, the nursing co-chair of the Rise program, and that stands for resilience and stressful events.
And this is a program that is a true peer-to-peer evidence-based program. So if you have a health care provider, it's In need if they have an adverse patient event, if they have a medical error, if they are struggling with a loss of a patient or loss of a coworker, they can simply pick up the phone and dial three peer and they can be connected to a peer supporter 24 hours a day, seven days a week.
So that is support that is available to them at any time. We also are in very close contact with our E. A. P. So, if we have a health care provider that we feel may need something beyond just a peer support, we have employee assistance programs, giving free counseling sessions, professional counseling sessions to our health care providers. We do have a program called Nurse to Nurse where we have nurse practitioners that are available to lend professional counseling support to our healthcare providers. So, it is a really exciting time to think that the holistic health and well-being other health care providers is in the forefront of Jefferson Health and many other organizations across our country. So that's really important for us to sustain that strong and healthy nursing force moving forward.
SARAH: And what about support for people like you who are supporting new nurses?
DEBORAH: So that brings us to the Pennsylvania Nursing Workforce Collaborative. So that is that extra level of support for us as residency coordinators.
And the wonderful thing about the collaborative is it does provide us with so many resources as coordinators. To support us, to strengthen us, to make us better at what we are doing. And then to give us so many wonderful different resources and supports to continue in this role. So, it was established in 2016. And that came out from a article through the Institute of Medicine to say, what can we do to support those people supporting our nurses? So, I can tell you the collaborative provides us are the coordinators across Pennsylvania with training and programs. We get communications, we get resource sharing, we have networking events, we have quarterly summits where we can hear about all the wonderful work that other coordinators are doing across the state of Pennsylvania.
So, it's really a wonderful resource for us and a wonderful way for us to share ideas and for us to grow our nurse residency programs.
SARAH: So, like, anything in healthcare and really probably all things should have this, um, but I know that Vizient really prioritizes that evaluation component. So how do we know that what we're doing, you know, we're doing well? How does the Nurse Residency Collaborative measure its impact with the new nurses, with the coordinators, and with the hospitals and health systems participating in a program?
DEBORAH: So again, you know, there are so many levels of evaluation, and I'll take you through. So, every time I give a nurse residency seminar, the nurse residents engage in an evaluation of my program.
Again, that helps me learn and grow my nurse residency program. And then through Vizient, our nurse residents are able to take surveys, through the Vizient database. So, the nurse residents take the Casey Fink graduate nurse survey and it's a survey administered, um, when they initially start the program at six months and then at 12 months and then Vizient then follows up at 24 months and then again at 36 months and it really is able to allow us to measure how the residents are feeling. What is their confidence level? What is their stress level? How do they feel about their overall competence in being a nurse? There are five areas of domains that we get some data on. Support, organization and prioritization, stress communication, and leadership. So, the nurse residents are able to on that four-point Likert scale to say how comfortable they are in all of these different domains.
So we're able to gather so much information through this, the Vizient surveys that we can, um, help. tailor our curriculum to. Vizient also allows us to give surveys to the leaders of our organization for them to give feedback about the program. We do that annually. And then again, we have that annual outcome survey where we're able to look at what is our retention. What is our turnover? How many nurse residents are in our programs? Where are they coming from? What services? And then when we think about, you know, what schools are they coming from, how are they feeling related to the information that we get from the Casey Fink surveys, the progression surveys, and then again, at the end of the program, the nurse residents complete an end of the program evaluation that allows us and gives us a summary of our program.
And then when we think about. our collaborative, we are evaluating all the work that we are doing across the Pennsylvania Nursing Workforce Collaborative. So, we evaluate all of our in-person summits that we attend. We evaluate the collaborative through a nursing needs assessment from the collaborative.
So, we did reach out to our collaborative and said, what are you looking to the collaborative for, what areas. So, we are working on a few initiatives through the collaborative from our needs assessment. And we're really, really thrilled about that. There is a return of investment calculator that many of our collaborative members were very interested in being a part of. We're really trying to tailor all of our summits and meetings at a time that really works well for our collaborative members. So again, many, many layers through nurse residency, through Vizient, through the PA collaborative that we are constantly evaluating our programs to make them the best that they can be because they are serving our nurses who and then serve our patients and you know, that's how we're going to get those positive outcomes at the bedside if we support and do all we can for our nurses.
SARAH: So, with that in mind, what excites you when you think about the future of healthcare and the future of nursing going forward? What gives you the most hope?
DEBORAH: This is a profession that is so near and dear to my heart, but I really think that there is so many opportunities and great potential for personalized care. preventative medicine through the technology advances, through AI, through all of the predicted analytics that we have in healthcare right now.
So many wearable devices for our patients, which is great because we can identify their challenges and their health status in real-time. And this will really allow for us to have better-targeted treatments. for our patients so they can have better outcomes. But again, you know, for the nursing profession, I think what's exciting for us as nurses is that there are so many opportunities for nurses. So many opportunities to work at the bedside, to work in specialized areas, to work in ICU areas, to work in outpatient areas, to work in clinics or work in schools, so there is always a place for a nurse to call home. So, you know, I started out in surgery and trauma, and then I've gone full circle to work in nursing professional development and work for those new-to-practice nurses.
So, there's always something exciting for you as a nurse to do. There's always a way to learn and grow every day.
SARAH: As we come to a close, do you have any final thoughts you want to share with our listeners?
DEBORAH: Working with those new-to-practice nurses is an honor and a privilege to me. I tell them every single day three things.
I say to them, you need to show yourself some grace. You are learning an awful lot every single day so do not be too hard on yourself. The second thing I tell them is, you know, important for them to take their lunches and their breaks, that they can't take care of the patients if they don't take care of themselves. And then finally, I always say to them, nursing is a very, very tough job. So you need to make sure you are doing something for yourself every day to fill your cup up, whether that is taking a walk, or riding a bike or reading a book or even just sitting on the sofa or exercising. Whatever is going to fill your cup up, you need to do that because in healthcare, you cannot let that cup run dry.
SARAH: Thank you, Deb, for coming on At the Core of Care with us. It was such a pleasure talking with you.
DEBORAH: Thank You.
SARAH: We're going to close out this show with a final thought from Anita Baldoni about what gives her hope for the future of the nursing workforce and the future of health care. Anita works as the nurse residency coordinator for Geisinger Northeast and she's a part of our Clinical Faculty and Preceptor Academy.
She's participating in our Academic Publishing and Dissemination committee.
ANITA: It is so exciting to see our students in the local academia preparing for their careers in healthcare and in nursing. They are so empowered, they are so autonomous, and they are so excited to make such a meaningful impact on our community.
and all of our patients. And it is really, really exciting to see how excited they are and how willing they are to go the extra mile and to take on so many different challenges in academia to put themselves out there and to be a part of this great, great career in nursing. I'm super excited to be a part of it. And I'm so happy to see our future grow. So many great resources are coming available as well. So much new technology and virtual reality, so many different educational tools to help our future nurses succeed. And I'm super excited and proud to be a nurse.
SARAH: Special thanks to Deb Gardner for joining us. And to all the members of the Pennsylvania Nurse Residency Collaborative for their dedication to supporting new-to-practice nurses. Thanks also to Bianca Innaurato, Brianna Blackburn, and Anita Baldoni for sharing their thoughts with us about the future of nursing and healthcare.
You can find our most current and past episodes of At the Core of Care wherever you get your podcasts or at PANursingWorkforce.org. For more information about upcoming webinars and trainings where nurses can obtain continuing education credits, log on to PANursingWorkforce.org or NurseLedCare.org. On social media, you can stay up to date with us through our handle at PANursingWorkforce.
At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder. I'm Sarah Hexem Hubbard of the Pennsylvania Nursing Workforce Coalition and the National Nurse-Led Care Consortium. Thanks for joining us.
SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families, and communities. I'm Sarah Hexem Hubbard with the Pennsylvania Nursing Workforce Coalition, and I'm the Executive Director of the National Nurse-Led Care Consortium.
I'm excited to share with you that we recently underwent a brand refresh. We previously went by the Pennsylvania Action Coalition, and now we're the Pennsylvania Nursing Workforce Coalition—a new name to make our state's nursing workforce front and center. As part of a five-year strategic plan, we will continue to advance, support, and advocate for a nursing workforce that helps create a healthy Pennsylvania through equitable, high-quality, and safe nursing. And to implement our mission and vision to advance nursing and create a culture of health. We've established three core initiatives. They include bolstering nursing workforce pathways, reimagining public policy through data, and embracing diversity through equitable solutions. Joining me on this episode to talk more about our strategic priorities, as well as trends around the future of nursing and healthcare is Daniel Hudson.
Daniel is one of our newest advisory board members. He's the vice president and associate chief nurse executive for nursing operations and administration at Jefferson Health in Philadelphia. Which is now a 32-hospital integrated health system across Eastern Pennsylvania and Southern New Jersey. Daniel, welcome to At The Core of Care.
DANIEL: Thanks, Sarah. It's nice to be here with you.
SARAH: So, before we really dig in, can you tell us briefly, you know, why you chose nursing as your career? How did you get into it?
DANIEL: So, my story about how I got into nursing is not the typical story or journey. There’s actually no nurses or healthcare providers, even in my family.
Immediately speaking, and I had chosen to go premed right out of high school. And the reality is not that I wasn't happy or unhappy with premed, but the school that I had chosen, I was very unhappy about, which led me to go home. And on that Christmas break, I was sitting on the couch. I can go back there to this day talking to my mom and I was crying. And I just, I didn't know what to do because I didn't like the school that much. And my mom convinced me. She sat there and she said, you know, maybe you should try nursing. Maybe you should stay close to home and try nursing. And I kind of looked at her and I was like, well, what's nursing? I don't even know what that is. But I knew I liked science. I knew I liked math. I knew I liked the human body anatomy, things like that. And I knew I liked to just serve people. And so not really knowing. Uh, what nursing was my mom convinced me to take that track. She actually helped me complete my application and I will never forget. I had gotten into two local schools. One was an ADN program, like an associate degree. And the other was a four-year BSN program, but I was on the waitlist for the four-year one. And. My mom called them and she was asking them all these questions. One of them was the final question of, well, how many, how many men do you have in your program that's starting in this upcoming semester?
And I remember hearing her response saying, well, that alone's a reason to get him off the waitlist. And so, um, one thing led to another in that next semester. So, we're talking in a two-and-a-half-week period. I was now enrolled in a four-year nursing program, and I still didn't know what nursing was about. But I found out in my first clinical, what nursing was about, and immediately I fell in love with it. I just love the idea at that time of serving people in such a personal way. And that idea really resonated with me from a core value standpoint. And so I got through nursing school and I did my nursing residency at Vanderbilt and from there I went on to pretty much do about every type of clinical nursing you can probably think of until I transitioned into leadership around 2008. So not the typical story, but it's my story.
SARAH: We often talk about nurses as advocates, and I, I like your story because it's about mothers as advocates too, right, um, paving the way. So, now we've heard a bit about your nursing story. Tell us a little bit about the health system that you work for now, and what's your day-to-day role?
DANIEL: Yeah, so our system, as you noted, newly cemented 32 hospitals, so we are a growing, integrated healthcare delivery network. We now are one of the top 15 nationally ranked integrated health delivery systems with a total revenue of a little over 14 billion dollars. So, we are big. We serve communities across 32 hospitals, 360 sites of delivery across a large portion of southeastern Pennsylvania, and even portions of western New Jersey. And a part of that is that we serve a wide span, and we can do that with a more than 12, 800 nurses and more than 7, 800 physicians. And additionally, what makes us unique is that our system has a university with more than 9, 400 plus students and a healthcare plan that ensures over 360, 000 members. So, we are this gigantic care delivery system now, but we really believe because of the uniqueness of how we're set up within the communities that we can still be local. Which is really important. And then the question is my role within all of that. So currently I remain focused on what we call legacy Jefferson Health right now. So that's 16 hospitals on the Jefferson Health side prior to the merger. And that accounts for a little over 400 total care sites and a little over 9, 600 nurses.
I've been in my role for about two and a half years here at Jefferson, and I describe my role in three big buckets of work. The first bucket is building robust talent streams or care pathways, effectively and safely using our resources is the second bucket, and the third bucket is investing in and engaging our people. And so when you think about those three kinds of buckets on a day-to-day basis, I have a very strategic relationship with the Jefferson College of Nursing and other local community schools. In the Philadelphia region to build those pathways to set up apprenticeship programs is an example, whether you're a rural hospital, that's critical access, or whether you are a freestanding academic medical center, or whether you are an integrated healthcare delivery system, you can take these things. If you're doing them in the right way and the right method and in the right timing and scale it up and down and it really works. I also kind of oversee all the fun stuff with budgets and finance and Excel sheets and capital funding. Usually, when nurses don't like to get involved in, but again, as I shared, I like math and I like numbers. And I also kind of oversee some of the care delivery transformation work at Jefferson Health, how we're implementing virtual care nursing and thinking about our care models very differently, and all the flexible teams that we have in our staffing offices. And finally, in that investing and engaging our people, I am one of the executive sponsors for our nursing professional governance structure that we have at our system level, as well as our nursing leadership development program.
SARAH: What made you want to become involved with the Pennsylvania Nursing Workforce Coalition's Advisory Board?
DANIEL: I've been involved in nursing workforce operations now from like a strategy type perspective for a little over 10 years. I've seen the good, the bad, the in-between of this work, and I really want to ensure that we have the right people taking care of the right patients together as a strong, effective team. And that's my goal, whether it's doing that work for Jefferson Health. Doing that work on other boards in the community or being an advisor on boards. Another thing I think is I see we still have so much work to do to improve the environments in which our nurses and our staff are providing care. We've come a long way. But we've got a long way to go and systems remain cumbersome and very complex. I mean, we've talked about how big Jefferson is. We're very complex. And my passion is really to help evolve and grow the systems, including our people. I think of myself as kind of being a nurse to the nurses.
And so, I see the advisory board as a place to influence change at a larger scale, not just for Jefferson Health, but also for our Pennsylvania communities as a whole. And the coalition has already done some fabulous work, really important work. And now I believe it's the time with this refresh to really push the boundaries and continue to evolve how we collectively think about building our profession for the better of our community.
So, I see this as a great way to do all that.
SARAH: So, let's dive in now to talking about our three core strategic initiatives here at the Pennsylvania Nursing Workforce Coalition. We're going to start with our goal around bolstering nursing workforce pathways. So, Daniel, you just told us there are more than 12, 000 nurses’ part of the Jefferson Health System across 32 hospitals. That's a substantial workforce, just at Jefferson alone. Can you share with us some specific programs and initiatives that you're working on? Related to recruitment and retention.
DANIEL: So healthcare is complex. So, I'm going to try to keep this at a high level and explain it in a simple way. And so, we're going to break that building robust talent streams into two areas of focus.
And the way that we think about it is new to practice and experienced from a recruitment standpoint in particular. So, from the new to practice standpoint. As I mentioned, we have a university as a part of our integrated care delivery system, and we have one of the top nationally ranked nursing schools in the nation. Actually, that was something that came out in the last couple months. So, we've done a lot of work collaborating with the Jefferson College of Nursing to build programs that better prepare our new-to-practice nurses as they enter the profession. So not only are we providing locations for the clinical rotations themselves, we have a very extensive capstone program that offers students positions during that final clinical rotation. So, what this does is move the recruitment process up quite significantly. And it really shows that we have an ability to capture more of our Jefferson College of Nursing students. To enter into our healthcare system who we've invested in. We're able to hire around 50 percent of those nurses of the total graduating nurses every year.
So, what that means practically is that every year Jefferson is hiring around 250 to 300 new to practice nurses from Jefferson College of Nursing alone. And that's not even with the other colleges that we have strategic partnerships with. Additionally, we've done things like build apprenticeship programs for other hard-to-fill roles like surgical technicians. To do that, we leveraged a partnership with an external vendor, and they provide the didactic for that apprenticeship training and we hire those individuals, and they are employed by us while they're doing their clinical required. hours as well. So, it's a true apprenticeship program and we invest in that, and it's been highly successful. We've hired over 60 surgical tech apprentices in the last two years since we've launched that program. And more recently we've began to explore strategic partnerships with other local technical and community-based schools that we can continue to bridge that gap for both nursing and allied health professions.
And we really are passionate about really working with schools that are in our communities and build our diversity pipeline so that we have our people serving our people. And we'll talk about that a little bit later. So, when we talk about experienced nurses, we've invested in a good amount of resources, both people and dollars around advertising and innovative technology that helps us recruit experienced nurses. We've also built internal flexible teams like our nationally recognized SEAL team that attract experienced talent because the work. that they get offered is flexible, it gives them really good pay compensation, and it gives them the ability to work in many different care environments. And we're really learning with the newer generations and the younger generations.
SARAH: Can you just for our listeners clarify what the SEAL program is?
DANIEL: Yeah, Sarah. So, thank you. So, our SEAL program that stands for service, excellence, advocacy, and leadership. And that is our system based. We'll call it loosely Float Pool team that are our nurses that go across all three of our regions and all currently 13 of our hospitals so they could work in Center City one day. In Philadelphia and the next day, they could be up at Einstein and then the next week they could be over in New Jersey and then the next week they could be up in Abington. So, they are really flexible and they're really moving all around this system and we deploy them in a weekly basis for the majority. So, as I mentioned we focus on investing in and engaging our people. That was a big bucket of my work that I mentioned. And this one has been let's call it difficult over the last five years as we've been coming out of COVID. And I think that Jefferson done a pretty good job investing heavily in development programs, clinical advancement programs, wellness, and wellbeing programs, but it doesn't stop there. Jefferson invested over forty million dollars last year in our fiscal year. To give our nurses and all of our nursing staff. So patient care techs, unit secretaries, monitor techs, all of them, an additional 5 percent raise over the annual 3 percent raise. So, in a six-month period, they got an 8 percent raise over their base salary.
We really believe that was the right thing to do. And it was really focused on retention. We wanted to retain the knowledge and the skills within our system because we know that the city of Philadelphia, in particular, is highly competitive and nurses are working full-time jobs at one place and per diem at another place. And so, we really wanted to make that investment. And here at Jefferson Health, we also have an extensive clinical advancement ladder that incentivizes engagement and incentivizes career development, and it incentivizes growth on top of their base salary. We also have nurse leaders solely focused on well-being and wellness programs. And we also recently refreshed our system nursing professional governance structure to align better and connect to our regions. And that's really our structure where our nurses have a voice and decision-making around policies and procedures and the profession and how that translates at Jefferson Health. So that's just a little bit about recruitment and retention.
SARAH: And I think what we hear from, you know, nurses across the state is that it's not going to be any one solution. You sort of need all of them. For some, it's compensation. For some, it's advancement. For some, it's flexibility. Um, and really, really being tuned in to what the needs are, and the interests are. How about mentorship? We hear a lot about that, especially, and I know we'll dig into this more later, related to diversity. But how do you support mentorship and networking across the system?
DANIEL: We have several ways we do that for our new-to-practice nurses in particular, we invest in nurse residency programs. And so, across all of our hospitals, we have nurse residency programs that have mentoring built into those programs where they're coming together. They're sharing about their experiences. They're talking about different aspects of either our core values. Or professional topics like medication safety, for example. So, um, that's one way for new to practice in particular. The nursing professional governance is another way where that networking really comes in, right? So, we launched a system structure just very recently, a refresh of a structure we had in place. And we were very intentional on simplifying it and ensuring that the campus Councils in the system councils, same language, same purpose.
So, for example, we have a system council that is called the professionalism Development and Advancement Council. So, we have that at the system level, and we have that at each campus level, and we even have the chairs from the campus level ones that sit on the system one. So, you can see the intentionality of creating ecosystems within our macro ecosystem, right? And making those networking connections because it's about decision making, improving our profession, but it's also about sharing knowledge and cross-pollinating all of our work and experiences. So those are just a few ways. We have professional development programs for our nurse leaders too. We don't want to forget about them. And we're really intentional around bringing together, we have an all-nurse leadership forum that comes together quarterly for all of our nurse leaders. And we're thinking and being smart about those kinds of town halls, we'll call them for our nurses and our nursing staff, where they can talk with our executive or senior leaders and not just talk with them, but there's back and forth and they're sharing ideas.
So, lots of ways to create that networking and mentoring.
SARAH: Yeah, and I'm hearing a lot of creativity in terms of how to take a really big system, um, and drill down a little bit to create those, I think, ecosystems within the system, which is a really interesting approach. So on the flip side, and you had mentioned, you know, some of the challenges of the past five years, but, you know, thinking about the rapid growth of even [00:18:00] just the past year, Looking at the diversity of systems that have joined Jefferson, what are some of the challenges that you're seeing related to recruitment and retention?
DANIEL: As we continue to grow its large healthcare systems, right? That's kind of what we're seeing going on nationally. It's not just in Pennsylvania. It's a national trend that's going on, and there's lots of reasons why. But it creates lots of complexities, lots of ecosystems within ecosystems. And I would say that the culture is probably one of the biggest components that creates challenges to recruitment and retention. And just overall, just it creates challenges. I think about little things like people wanting to hang on to the name of their hospital and what it was called because they have an identity in that and in the community in which they're serving as well. They are attached to that identity, and it's been around for in sometimes 100 years even. So, thinking about how you take the good of that culture and weave it into the larger culture is work for you. That's ongoing that we're always thinking about and we're always focusing on. We really want to build an identity and we've been very intentional at Jefferson Health around what is our identity and honestly, what is our nursing identity?
We're in the midst of that work right now, even as Lehigh Valley is merging into Jefferson Health and thinking about, well, what is the nursing identity at Lehigh Valley? What is the nursing identity at Jefferson Health? What are the commonalities so that we can speak the same language and begin to form a common identity? I'd say another challenge, not so specific to a large healthcare system, certainly, this would apply to even a freestanding medical center, is medical surgical nursing. It has become one of the biggest challenges where we are seeing an average tenure of only around two and a half years within Jefferson Health. And you can sit and think, wow, well, that seems good when I hear about turnover. But the challenge to that is the majority of our beds and acute care are medical-surgical beds. And so, the skill and the competency is constantly in flux. And so, we're currently engaging our nurses through folks groups and different things to try to understand, well, what's driving this phenomenon? Why do nurses want to go on to be in ICU or ED or some other specialty? And is there anything we can do to increase that tenure in medical-surgical nursing specifically? And I'd say finally, patient care technicians, we talk a lot about nurses. You hear all about the challenges with the nursing are in workforce.
There's a challenge with patient care techs too. And one of those challenges is the reality, we're competing against Starbucks and Target when it comes to wages and benefit packages. And working at Starbucks is a little bit easier than working in a medical surgical unit in a hospital where we see patients and patient families being more aggressive towards the staff. And so, we're doing a lot in that arena as well. In the past year, we actually created a career pathway for patient care techs by upskilling them. And through that upskilling, we created a whole nother wage ban for patient care tech. So we have like a patient care tech one and a patient care tech to role. And so that's just one practical example of how we're trying to tackle both the PCT challenge, but also the medical surgical challenge. Even the identity piece of the work.
SARAH: And I appreciate that in talking about the nursing pipelines We are talking about other health professions. Even your own story of training in medicine and then moving to nursing um so really looking at the whole of the health system and not these individual parts as part of looking at those pipelines. So, let's move on now to our second core strategic initiative, which is reimagining public policy through data
In this area we want to increase access to data, improve data literacy and drive more informed statewide policy. We want to shift narratives with patients, advocates, and educators. It's healthcare institutions, government officials. We've certainly been doing work in this space, um, largely as a neutral convener, really trying to bring people together, sharing different perspectives, but we really want to center data in those conversations. So just to get us started, do you have any personal stories to share about your own practice and how maybe that shifted to policy?
DANIEL: One that comes to mind is work that I've done prior to me moving down to Philadelphia and working for Jefferson Health. As I participated on the Organization for Nurse Leaders Legislative Committee, and that's the professional organization for a group of states in New England, actually, that aligns with the American Organization for Nurse Leaders. Before that, I was a Vermont State Rep. On their board as well, and then transition to this legislative committee, and we did a ton of work supporting through evidence and data developing bill language that could be used to advocate at the state level for building pipeline funding for nurses in the state of Vermont.
That was a great, great example that I can think of my own personal story, and I also think of an example that comes to mind. Uh, when I participated in the American Organization for Nurse Leaders Advocacy Day, which is right in Washington, D. C. So that was a couple of years back. And I had the opportunity to speak with congressmen and congresswomen about increasing the healthcare workforce and protecting healthcare workers. And for all of those Bernie Sanders fans out there, I got to actually meet Bernie and talk with Bernie. Because he was, at the time when I was in Vermont, our state, well, still is our state representative, uh, Senator, but, uh, it was a pleasure to get to talk to him and share some of what the work he does and some of Peter Welch and other representatives in Vermont can do to help us from a nursing standpoint.
SARAH: So, from your perspective as a nurse executive, and I mean, as a nurse, what are some ways to have nurses get involved to be more active and inform statewide policy?
DANIEL: Well, generally, I think. The first step is just learn who your local state senators and representatives are. You should know that. Just got out of election season, so hopefully it's fresh on the mind. You know, and when there's an issue to advocate for, or there's something that you think that you're very passionate about, contact their office. Many of them make it very easy to just email them, email the legislator and their staff directly, send a query online, offer to meet with them to share your professional perspectives, which can actually be more impactful than you really think. And when you do that, not if, but when, really encourage you, tie it to a patient or a staff member story that's really relative to that issue at hand. You know, some examples of things you might want to write to your legislators are about, around staff safety, addressing nurse faculty and clinical site shortages, increasing the healthcare workforce, all the things that Sarah and I are here talking about. I'd also say, again, simple things here, practical and simple, to sign up to receive email updates from them and from your professional organizations. We're all members of professional organizations, whether it's leadership or just at the staff nurse level, or even outside of nursing. There's lots of professional organizations for respiratory therapists and physical therapists and occupational therapists, the list goes on.
And they all have their advocacy priorities that they have every year. You can go right onto their websites and go look them up, or you can sign up for those emails so you don't even have to go there. They just land right in your inbox. And I'd say get involved with your professional organizations. They really have these priorities. They have tools. They have resources. They even have templates that you can pull up, type in whatever you want to type, and then send that to your local senators or state representatives. And I'd say most importantly, don't think a conversation with your representative doesn't matter, or an email doesn't matter, because it does. It really, really does. So, I would say to sum that up, be intentional and take small steps, but take those steps.
SARAH: Yeah, and I really want to underscore what you were saying about, you know, don't underestimate your expertise. What I hear often from nursing students in particular is that they don't know what policy is, right? That's sort of a foreign area. And that's very problematic when it comes to creating a good policy, but also such a miss because there's so much information on that nurses have. And there's so much trust that nurses are able to, um, transfer, right? From the stories that they're, um, collecting and learning from, um, and to share those stories. There's a lot of trust in that and a lot of power in that. So, I appreciate you, you calling out how much nurses really do have to add to the conversation. So, we're going to move now into our final core strategic initiative. And now's as good a time as any to talk about how, um, our initiatives are really structured in a um, circular way because they're all overlapping.
They're all intersecting and you really can't do one area without another. But in this, uh, strategic initiative, we're looking at embracing diversity through equitable solutions. So again, Daniel, you're looking at quite a large system, a huge population of even the people who work for Jefferson, and then an even larger population of the people that Jefferson is serving. Share with us some of the ways that Jefferson Health is approaching diversity, uh, working to increase diversity in the nursing workforce and improving care delivery.
DANIEL: And we know, Sarah, that this is a topic that means a lot. It goes deep for a lot of people, and I say that because I just want to underscore how important it is.
As I mentioned before, and this might sound a little strange, but as we started to create that flexible RN SEAL team that I talked a little bit about. We really intentionally thought about diversity as we were building that team and the data kind of shows that. Out of our 140 RNs that provide care across our three regions on that SEAL team, 41.4 percent are underrepresented minorities. So, when you think about that, this is compared to a benchmark of around 28. 2%. So, we've almost doubled the benchmark from a diversity standpoint of the 140 nurses providing care across our 16 care sites right now. Additionally, that team is only, and I know I say only here, only 71.1 percent female. I know that sounds high, But when we talk about nursing, it's actually low, and that's compared to a national benchmark of 79. 1%. So you can see there that as we were building that team and being intentional about building that team, we were really thoughtful about the diversity we were trying to build into that team. And of course, that's not the only focus when we're hiring people and recruiting people. We're looking for skill. We're looking for the right fits, but it's an important variable. And I think that it shows that we're focused on that. Another area that we're really focused on in Jefferson Health within nursing is building strategic community partnerships.
We believe this is critical. We've partnered with local inner-city colleges that serve the underserved. One really practical example is we built a work-study program with an inner-city college that focused on entry-level positions like these patient care technicians that we have been talking about. And these students were able within their final year of high school to do a work study program as a PCT, which then helped them get into the local college. And then they got a job for us as a PCT. And so, you can see how that's really starting to serve our communities in which we're embedded. And I'll never forget the story I heard of one of the PCTs in this program recently. They shared that this PCT who is now in college So it's the first family member in college to go to college. It's also the first family member to hold a full-time job and get a real paycheck. And they shared how this paycheck now allows them to live in a more safe community, closer to where they work. And it's paying for the whole family to have an apartment. So, it's these types of, really personal impacts that we're having on our communities and it's in communities that are underserved and it's the type of investments that Jefferson Health knows we need to make, and I know there's other health care systems making these similar type of investments.
Finally, we're focused on embedding diversity and belonging into the core of who we are. And Sarah, you might say, well, how do you practically do that? The core of who you are, that sounds deep. Uh, well, one practical example is we went and looked at all of our job descriptions. And we made sure that the language within all of our job descriptions calls out the importance of having a diverse team that you work with and being competent and culturally aware of the different diverse individuals that we work with.
SARAH: And so how do you see, not just that example, but as a whole, how do you see those strategies translating into the type of care that's being delivered when we're looking at sort of culturally humble models of care?
DANIEL: I would say that it's good for someone who is sitting in a hospital bed. Or showing up to an ambulatory clinic and is really scared because they're there for the first time. How important is them to kind of see someone that looks like them, talks like them, and has some of the core values that they have. And so I think that's how it shows up is by our people looking like the people that we serve, at a very high, high level. I would say there's other practical ways it just shows up, right? So, at Jefferson Health, we have an extensive program around our patients having the ability to have translation services across ambulatory care sites, our urgent cares, and in our acute care hospitals. Extensive. It also shows up where we start thinking about, okay, we're going to have a clinic in a community, and we have to understand that community's cultures.
And this is a true story at Jefferson Health. We built a clinic, and the local community was afraid to actually go into it. And we did a lot of research, and it was because of the colors of the walls. And so that's how it shows up, right? We [00:33:00] had, if we would have known and done the right focus groups and done the right work up front, we wouldn't have painted the color of wall that we colored to open that up. And so easy fix. get that changed, and then we're able to really, again, practically just invite our communities into our different care sites to be able to provide the right care for them. So those are a few different examples. I also think it's really important, and we're doing this at Jefferson Health, to invite our patients onto committees. And have them be a part of decision making around policies and, right, finalizing job descriptions, things along those lines. Patient advisors are critical to the idea of how we're going to foster culturally humble care across our care sites.
SARAH: As we think about these initiatives and the role that the Pennsylvania Nursing Workforce Coalition can play, you know, we talk a lot about creating spaces for learning and to think about the sort of sustained impact, the collective impact of having those kinds of spaces. So as an advisory board member, what excites you about these opportunities?
DANIEL: Well, here at Jefferson, Sarah, our mission is to improve lives together, and I want to call out that word together. And so that's what really excites me about this opportunity. It's the together part. It might sound a little cliche. I know that. But it really is foundational to improving the lives of our communities. Like we have to do it together with them and with each other. So through a strong coalition that has like-minded individuals, like-minded mission, and focused on people and organizations that are part of our communities, I think we can make a difference as we're working together. We're making a difference as we continue to bring all of us together, share ideas, cross-pollinate. There is power in size. When we think about it the right way, and we do it the right way. So I really believe that's the power we have to forge together and chart our path forward.
SARAH: I think that's really well said. And, you know, looking more broadly at the future of what we do together, what excites you about the future of healthcare, the future of nursing, the future of healthcare?
DANIEL: I'd say, Sarah, that I have hope for health care. There's a lot of challenges right now. There's a lot of financial forces. There's a lot of regulatory headwinds right now for all of us.
But I also would say that it's in those challenges, and I know we learned this through COVID, we've even learned it through the most recent IV, uh, fluid shortage. It's in those challenges when we actually are forced to come together to think about how we're going to get through this together, because when everything's going great, we're over here on our islands and we're figuring it out by ourselves. But I really think we're an environment that's pushing us to think about how we do things together more and more and that that does excite me when I'm out there talking to nurses who are caring for our patients. They share stories where they're hopeful the world's not ending and health care is not falling apart and they're working together as teams even though the environments are challenging and they share stories of how they're going above and beyond despite you know all the workplace safety issues and let's call it what it is we have staffing challenges across the whole health care delivery system. Do we have a ton of work to do? Absolutely! Are we engaging the right people to help drive the change I think that's the question and I believe that we are.
And building coalitions like this and working together.
SARAH: So before we wrap up, do you have any final thoughts you want to share with our listeners?
DANIEL: This might sound cliche again, but it's simple, but it's impactful. I really encourage everyone to just start somewhere. That could be an email to a colleague, a Google search on how to recruit, uh, using innovation, like Google AI these days. Just try it out. Just be intentional and keep taking steps. You don't have to eat the whole elephant at once. You just need to take one step at a time. And you need to be able to encourage yourself to take a few risks. Just take a few risks. We don't evolve as humans without taking calculated risks. We all do it every day, whether we like it or not. You drive on the highway, you're taking a calculated risk. And finally I would say, as you're starting somewhere, just extend grace. This world needs so much grace right now, and it starts with me, starts with you, Sarah, and it starts with all of our listeners.
SARAH: Daniel, thank you so much for joining us on At the Core of Care. We are so excited to be working with you on the coalition.
DANIEL: Thanks, Sarah. It's been a pleasure to be able to spend time with you and share a little bit about our experiences at Jefferson, and hopefully, it's been helpful for our listeners.
SARAH: Special thanks to Daniel Hudson for joining us. And to all the members of the Pennsylvania Nursing Workforce Coalition's Advisory Board for their dedication and guidance as we mark this new and exciting chapter for our work. You can find our most recent and past episodes of At the Core of Care wherever you get your podcasts or at panursingworkforce.org. For more information about upcoming webinars and trainings for nurses to obtain continuing education credits, log on to nurseledcare.org. And on social media, you can stay up to date with us through our handle @ nurseledcare. At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder.
I'm Sarah Hexem Hubbard of the Pennsylvania Nursing Workforce Coalition and the National Nurse-Led Care Consortium. Thanks for joining us.

On September 26, 2024, the Pennsylvania Nursing Workforce Coalition (formerly known as the Pennsylvania Action Coalition) hosted a successful and engaging breakfast at the 2024 Pennsylvania Organization of Nurse Leaders (PONL) Annual Leadership Conference in Harrisburg, PA. The pre-conference event marked the unveiling of the PA Nursing Workforce Coalition’s (PA-NWC) new strategic plan and the introduction of its key initiatives, aimed at advancing the nursing profession in the state.

The breakfast event featured a presentation from the PA-NWC Team that informed and inspired attendees, with a strong focus on the PA-NWC’s new strategic direction. The PA-NWC emphasized its commitment to three major initiatives:
The presentation received positive feedback, with participants finding the information valuable and relevant to their professional practice. The variety of speakers and perspectives contributed to a well-rounded discussion.

A highlight of the event was the interactive roundtable discussions, where attendees shared insights and ideas to enhance the Coalition’s initiatives. Roundtable discussion topics included:
Reimagining Public Policy through Data: Attendees discussed ways to integrate nursing into public policy by creating annual “state of the state” reports and expanding engagement through community events like health fairs and schools. Ideas also included introducing policy education to nursing students and mentoring leaders to run for public office, ensuring that nursing professionals play an active role in shaping policy.
Bolstering Nursing Workforce Pathways: Discussions focused on strengthening the nursing pipeline through youth engagement programs, such as Geisinger’s Aim HI and Allegheny Health Network’s Young Scholars. Participants emphasized the importance of providing financial support, internships, and clinical opportunities to students, while also addressing barriers like limited rotations and nursing school closures.
Embracing Diversity through Equitable Solutions: Roundtable discussions emphasized the need to build a diverse and equitable nursing workforce. Attendees highlighted the importance of engaging underrepresented communities through local organizations, schools, health fairs, and churches to raise awareness of nursing careers. Mentorship was also seen as key, with participants advocating for more support for individuals from diverse backgrounds in nursing education and practice.
 Suggestions included partnering with academic institutions to create programs that support underrepresented students and offering scholarships, internships, and financial support to attract diverse talent. Participants also noted the need for inclusive environments in both educational and clinical settings to retain diverse nurses.
Suggestions included partnering with academic institutions to create programs that support underrepresented students and offering scholarships, internships, and financial support to attract diverse talent. Participants also noted the need for inclusive environments in both educational and clinical settings to retain diverse nurses.
Networking and collaboration were central to the event’s success, with many attendees expressing that the interactive and community-driven format allowed for valuable exchanges of ideas. The Q&A session sparked engaging discussions, further enhancing the event’s impact. Overall, participants felt the event provided not only valuable insight into the PA-NWC's future but also a forum for fostering connections and advancing the collective goals of the nursing profession.
SARAH: Sarah, this is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families and communities. I'm Sarah Hexem Hubbard with the Pennsylvania Action Coalition and the Executive Director of the National National Nurse-Led Care Consortium. On this episode, I sit down with Donna Bailey, the CEO of Community Behavioral Health or CBH. They're the organization that pays for behavioral health treatment for Medicaid recipients in Philadelphia. We'll discuss how CBH supports mental health care and access to resources for many Philadelphians, and specifically how that support reaches people who are pregnant and parenting.
This conversation builds on some of our earlier episodes, where we talked about a mental health collaboration that NNCC developed with Joseph J Peters Institute or JJPI. Through that work, we've been able to support more than 200 clients who are pregnant or parenting young children to connect with therapy services. We've been able to sustain this type of community-based integration, partially because JJPI is part of CBHS provider network.
As you'll hear throughout this episode, access to mental health treatment is all about meeting people where they are and even engaging them in services before they need them. When it comes to systems change, we'll talk not only about innovations in overcoming barriers to treatment, but also, the social structures that impact mental health and well-being. What we know is driving most mental health concerns the social determinants of health.
Before we turn to my conversation with Donna, it's important to note that we're bringing you this conversation to coincide with black maternal mental health week, which this year 2024 runs from Friday, July 19 through Thursday, July 26
Donna, thank you so, much for making the time to be here today to have this conversation before we dive in. I just wanted to hear a little bit from you about what led you to get into community health and public health more broadly.
DONNA: Hi, Sarah, it's so, good to see you, and I just want to thank you for reaching out to give me this opportunity to highlight all the good work that's happening at CBH, and also, to highlight black maternal mental health week. So, in terms of my career in public health, to be honest, I have to say, this isn't the career that I envision. I was definitely off on a track for corporate work, and had actually worked at Johnson and Johnson for a little bit after I got my MBA. So, I like to tell people that this work really chose me, and I'm really grateful for colleagues and mentors who recognize my potential to serve and make a difference in this sector. So, sort of life circumstances, geography, I moved around for a little bit, and once I landed back in Philadelphia, decided that I was going to go get a second master's, this time in psychology. And so, after I got that degree, I started to work at nonprofits here in Philadelphia, did a lot of direct service work, kind of went up the trajectory and that ladder, and then realized that I could potentially be more impactful at the systems level. So, I got involved in government, and through that work, in 2013 landed at CBH for the first time. And so, I would say, through all of those sort of twists and turns, the common theme has been really being involved in work that it had an impact on health and wellness for Philadelphians.
SARAH: We'll definitely want to circle back to different components of your experience. But I think before we go any further, can you explain to the listeners what is CBH.
DONNA: Absolutely. And you know, we do have a little bit of an identity crisis. Our name in itself, kind of suggests that we do direct services, and we don't so, CBH, or community behavioral health, is the Managed Care Behavioral Health Organization for Philadelphia. So, what does that mean in Pennsylvania, insurance for people who are on medical assistance is managed care, and it's in a program called health choices. So, whether it's a physical health MCO, or behavioral health MCO. It's all a part of the managed care system called health choices in Pennsylvania. And so, when Pennsylvania decided to go the managed care route, counties were given the right to determine how they were going to administer the program, and Philadelphia was the only county to decide that it was going to create its own entity. And so, they created CBH. What makes it a little bit interesting is that we're not government, but sometimes we are. The actual structural relationship is that we are a nonprofit. We're a 501, c3 under contract to the city of Philadelphia to administer the program. And so, where we actually sit? Within city government is within the Department of Behavioral Health and intellectual disability services. So, the state contracts with the city through DBH IDs, and DBH IDs then subcontracts with CBH. And so, our sole reason for being is to ensure that for Philadelphians, and again, we're pretty unique in that the work that we do is only for Philadelphia. For Philadelphians, our objective is to ensure that we have a robust network of providers, whether it's independent practitioners or the big hospital systems and everything that falls in between, to provide services mental health, substance use disorder, autism services, the whole array, we are required to provide access to members who need those services. So, we maintain the network. We do quality work, compliance work, fraud, waste and abuse, all of the things that you would typically think that your physical health NCO would be doing. We do it. What makes us a little bit different and a little bit more interesting, and I think special, is because of where we sit in our relationship to city government. We have really strong partnerships with other health and human services organizations in the city, like DHS, which is child welfare, like the health department, like homeless services, and what we find is our members, our CBH members, our beneficiaries, are involved in multiple systems in Philadelphia. And so, through our work with these other systems, we're really able to treat the entire person. And so, these days, you hear a lot about social determinants of health. That's really what those other human services organizations are focused on housing, childcare, food access, pairing it with behavioral health really allows us to touch on all those things that really impact one's wellness. So, that's kind of what we do.
SARAH: Thank you so, much for laying that out for us, and you're right, it is complicated, but I'm definitely hearing some areas of opportunity in that structure. And you've been at CBH in your current role as CEO for about eight months, and then you were there several years before, but recently, and I know this from having the opportunity to work with you there, you were also, at Public Health Management Corporation for a while as well. How do you feel like your time doing some of that integrated health services work has impacted your return to CBH?
DONNA: That's a great question, and folks have asked me that as well. Even folks here at CBH are interested in what the lens is that I look through this work now, having had the experience at the provider level, but yeah, I was at CBH for about eight and a half years. I mostly served as the COO and then in 2019 when Joan Arnie was retiring, I was appointed the interim. And early in 2020 the world as we knew it changed, and we all pivoted, and remote work and telehealth, and all the things that we were able to dial into really allowed CBH to work with providers to maintain access. And so, during that time, I was thinking about what I might want to do next in my career. And I'll be honest, what I was really excited about when I was contemplating PHMC was the work that PHMC was planning at the Public Health Campus at Cedar, in collaboration with Penn and with IBX and with CHOP. And so, I started at PHMC in late 2020, as you said, as the chief integrated health services officer, and it felt like the lion's share of the services portfolio. So, I had all of the behavioral health and all the primary care services, and really my role was working with all of the leaders in those portfolios of work to figure out how we could streamline accessing services and receiving services for the member experience, so, that it wasn't disjointed or people weren't having to repeat things at intake. How do we look at the whole person no matter what service you're receiving? So, I think one great way that we were trying to do that was building out this Public Health Campus. And so, we had the federally qualified health center there, we had dental there, we had some of the other behavioral health programs there. And I think it also, stands as a really neat way to systemically begin to address health disparities. We know that that was the old Mercy Hospital that had closed, and there was a deep need in the community for services. So, really excited to have been a part of that project. But I will tell you I got, I think, a renewed sense of what some of the challenges are at the provider level, and particularly for direct care staff. And let's remember, many of us were able to work from home during those years, but folks who were tasked with actually meeting our members, they never stopped, you know, and telehealth was great, but for the most part. Start many services still occurred face to face, so, developed a real appreciation for that work, but also, for the work that organizations had to do in terms of envisioning what the future would look like, especially as we were coming out of covid and some of the resources that were available through the loans and other type of resources from the federal and state governments. As those were ending, agencies were really having to rethink their organizational structure, their capacity. You know, how people like to receive services was shifting. So, we were seeing drops in service utilizations, and all of it ultimately impacts the bottom line. I know we don't like to talk about dollars when it comes to health care, but it's certainly a primary component. And so, for me, I developed a real appreciation of what it takes to sort of manage the delivery of services at the provider level. So, I've brought that back here to CBH. And one of the things that we've really been trying to partner with provider organizations on are, you know, we ask for a lot of things administratively, and some of the things we're required to do, some of the things we ask for because we have an interest, we like to do surveys. So, we've really been trying to be thoughtful about, what are the things that we have to require of providers, because the health choices program requires it of us. What are some things that are informative and we should continue to ask for, and what are some other things that we really could dispense with? So, we're having those conversations with organizations, and I think they've been really fruitful. But for the most part, I'm really trying to reset the relationship that CBH has with the provider network, I really want it to be focused on transparency and accessibility.
SARAH: It must also, be really interesting coming back to CBH in this kind of returning into a different climate, a different atmosphere. And when you spoke about the government programs that have been dialed back over the years, we see that in the client and patient or member population as well, that potentially, some of the resources that were maybe lifting folks up during the pandemic are starting to go away. How is that playing out in the design of services right now at CBH looking to sort of the overall welfare of the community that CBH is serving.
DONNA: You know, there are services that we are required as a behavioral health managed care organization to pay for, and it's the gamut. I will say, a component of what we do in our provider operations portfolio is network adequacy. So, we're always looking at data to understand what utilization looks like in a particular level of care, and do we need more of something or less of something? And again, those are conversations that we have to have with providers as well, because we do believe there needs to be a resetting of the network generally. To your point that things are changing out on the provider landscape, some agencies are going to make the hard decision that they're going to close a program or reduce a program. So, we're working hand in hand to kind of figure that out. But I would say generally, we feel like we have an adequate network now. There are some services, and you know this, Sarah that there's always more need than capacity, particularly for children, and particularly for children who have autism. And so, for those services, we have what we call an open network, meaning any willing provider who can come forward and has been licensed and credentialed, we're willing to have you in as an in network provider. So, we're constantly looking at the data. We're constantly talking to providers. Increasingly, we're talking to members, so, we're creating additional opportunities to engage with members. We're going to be introducing, in the new year, a two-way texting program where we can follow up with members after services, to get a pulse on how did you like your therapist? Did you get in in the time that you thought you were going to get in? Tell us generally, what your thoughts are about your healthcare, and we're doing a lot more member education out of our Member Services Department.
SARAH: I'm glad you brought up network adequacy, because sometimes when we talk about access to mental health, people think about wait lists, but we know access is so, much more than that, and there are many reasons why people might not have meaningful access to treatment or just to the resources they need for good mental health. Can you provide some examples of how CBH is addressing access to mental health? And you know, once we've established network adequacy, what are the barriers, and how do we address those barriers?
DONNA: Sure, and I would say it's really all of those social determinants of health, transportation being a very basic one, child care, you know, if you don't have access to consistent and nutritious meals, the last thing you're going to be potentially thinking about is therapy. So, really, those basic, basic things that you need to just function. And so, one of the things that. We've been doing here over time, and I'm happy to share some of those with you. Today is really trying to meet members where they are. Our primary focus is offering member centric, integrated care. We have developed what we call our community-based care management teams, and that's exactly what the name says community. So, it's my trained clinicians, not working within the walls of 801 market, but being embedded in OBGYN clinics and children's hospitals and primary care clinics and federally qualified health centers. And again, they're not delivering services because we are the insurance company, but they are partnering with those community-based organizations and those primary care organizations to do a number of things, one education, because there's still a lack of understanding and a lot of stigma around mental health. So, they're there to educate the staff as well as patients. They're there to provide resources, referrals, linkages, and then they're there to actually talk to the members, you know, what are you needing in your life, to provide stability, to support your mental health? And then they can work with those organizations, with community-based organizations, with some of those human services agencies that I mentioned, to help navigate and to make those connections. And so, our overall goal for these community-based care management teams is really to reduce barriers address health equity, because we know underneath all of this is health disparities and health equity and really mitigate some of the social determinants of health barriers.
SARAH: That's so, essential in terms of reaching populations as a whole, and I know that we see this particularly in the perinatal population. I'm wondering if you could tell us a little bit about some of the initiatives that CBH is doing to reach that population.
DONNA: Sure. So, we have our integrated perinatal community care team, and they work specifically with this population, really as a preventative measure. And so, we know that women who are pregnant, women who are postpartum, are at high risk for anxiety, for depression, for a sense of isolation and feeling overwhelmed. And so, we wanted to work with other systems and with community-based organizations to try and get ahead and support women before any of those negative outcomes would happen. And so, this team is embedded in OBGYN clinics across the city, and essentially they are there to really walk folks through here are all the things that we could offer you, in collaboration with a food bank, with your primary care, with child welfare, and help them navigate those systems. One of the other really neat things about this team is that they have certified peer specialists embedded in the team so, women who have experienced some of the depression and anxiety that comes with being a new mom, and who have been a part of some of the human services systems and have had to navigate on their own, they bring a wealth of first hand information of all the things that they've learned along their own journeys. I would also, say another really neat feature of this team is that we have a pharmacist attached. And why that is important is oftentimes women are apprehensive to take medication when they're pregnant, specifically psychotropic medication for mental health disorders. So, the pharmacist is there to provide education, to work with the OBGYN to provide education as well around what medications might be safe based on the woman's health profile at that time. And we also, have a physician advisor, attach who is a psychiatrist who works in concert with the OBGYN. We've gotten great reviews about how this team has been collaborating in the clinics. We'd love to be able to expand, but we want to do some level of assessment, some lessons learned, be able to scale up strategically and thoughtfully. I'm really excited to report that since this program started in March 2022 we've worked with and enrolled almost 800 women, and what that means is that they've worked with our teams, and then refer to social determinants of health, communities, organizations or other organizations that meet their needs. So, we're really proud about that.
SARAH: Mental health is so, broad. We all know that it encompasses so, many things, what kinds of resources are available for parents who are experiencing substance use problems, and what kinds of services and resources are out there.
DONNA: I would say, even prior to the pandemic, CBH had really focused on reducing barriers to substance use treatment. Specifically, we knew that we were the epicenter of the opioid epidemic. Even today, Kensington is very much a focus of this administration. One. And so, we did a number of things, beginning in early 2020 late 2019 one, we eliminated any and all administrative barriers to getting into treatment. There's something in insurance called a pre authorization for services, so, to call the insurance company to get approval, we eliminated that for all substance use treatment programs. So, essentially, someone could show up at one of our crisis response centers, and in Philadelphia, those are typically the entry points for treatment, show up, be assessed, and be able to move right into a treatment bed, or show up at a substance use outpatient clinic and be able to start treatment right away. So, that was key, eliminating those barriers in terms of treatment beds Since 2020, we've also, brought up over 200 new beds again to make sure that we had capacity. I mentioned the certified peer recovery specialist. We worked with our state partners to make that a Medicaid billable service, and that's really important to be able to have Medicaid pay for as many services as we can. We've embedded certified peer specialists in ers and the crisis response centers, and we've done a lot of work with providers in particular to make sure that they haven't created any barriers to treatment as well, and so, we've asked them to look at their operational flow to make sure that people are getting through and getting the treatment they need as quickly as possible. We have 15 programs that are specific to women or women and children, which is really important to keep families intact. I want to call out a PHMC program, Interim House West for women and their babies, where they can get their treatment. They can study for their GEDs. They have groups. There's childcare on site. And so, we are really supportive of those types of programs that are treating women by keeping families together.
SARAH: And does that relate to Mommy's Helping Hands?
DONNA: Absolutely. Mommy's Helping Hand is another community-based care and management team specifically for women who are struggling with substance use disorder. That team is really tasked with coordinating care on their behalf, helping them schedule doctor appointments, education, connecting them to community resources, and just being that additional resource for a question, or how to navigate, how to get reconnected to a substance use treatment provider. You know, I've been disconnected, and I can't get an appointment. Can you help me? So, that's just another sort of tool and the toolkit specifically for this population.
SARAH: So, how does that look? I mean, how do you find these moms, or find folks that would benefit from this program?
DONNA: For mommies helping hand in particular, we don't contract with specific agencies. It really is outreach and engagement that our team does, so, they're cold calling agencies. Do you have someone who has this need? They do a lot of education with providers. We have oftentimes big provider meetings. They'll come and do a presentation. So, it's really us assertively outreaching to agencies that are in our network, other community-based organizations, really marketing this resource and this service.
SARAH: You spoke earlier about telehealth, and certainly, I think we all know the pandemic blew up our notions of telehealth and really rethinking access. So, I'm curious, you know, from your perspective, what does the future for telehealth look like, and also, what are some of its barriers? What are its limitations?
DONNA: Telehealth was really a godsend during the pandemic, and I have to say that our partners at the state really acted quickly and collaboratively to ensure that from a managed care organization, we were able to offer that as a resource. Even in the beginning, it was telephonic only, which is typically not allowed, and so, over the course of the years, telehealth has really been cemented as an option that we can all use to ensure that we maintain access. As a matter of fact, just this week, a bill passed in the Pennsylvania legislature really requiring managed care and commercial health plans to cover telehealth. Now, of course, we've been doing that here at CBH, but this is really a win for people who are medical assistance and people with commercial insurance. We were really delighted at that news. Now, I would say telehealth is not a panacea for everybody in every situation. Definitely was incredibly helpful when we couldn't be face to face, and there's certainly times when it makes sense. So, we talk a lot about transportation, But transportation is a very real barrier for a lot of people, and can make the difference between making the appointment or not so, great. In that instance, great when you don't have a couple of hours to try. Travel, but you could find a private space somewhere and do a telehealth appointment. But it also, has its downsides. There are times when therapy is more effective, when you can have that face-to-face contact. And so, for us, we are really looking for choice number one, that members have a choice, but that providers are offering the option, we get a little concern if we hear that a provider is not offering any telehealth and everything's in person, or they're only doing telehealth, and so, we're really expecting a balance that meets the needs of that agency's particular membership. I would say the other thing is that oftentimes, if you're trying to do a tele health appointment at home, and you're a mom and there's kids around, that could be distracting as well, and so, so, many different scenarios when it's the right thing, and at other times, an in person would be more effective.
SARAH: And centering that on the consumer's preference makes so, much sense. And I know we also, hear issues related to language access and even safety in the home, and really needing to make sure that we're meeting people where they are, wherever that is. So, this episode will drop during Black maternal mental health week in July. We know that an estimated 20% of new mothers experience a mental health issue, such as postpartum depression, but for black mothers, the incidence is much higher. One study found that it was up to 80% higher in a study focused in rural areas and small cities. But we would anticipate, I think, that being true here in Philadelphia as well. It's similar for a pattern of trauma exposure. So, a study that found trauma exposure to be the highest among black women, 87% for other women, ranging from 29 to 74% so, given that also, looking at associated risks, such as substance use disorder, seems really important that providers are recognizing the specific trauma that black women have experienced, and are continuing to experience, especially our perinatal population, that the instances that we're seeing so, much documented in the delivery of care. How is CBH looking at this issue and looking to address disparities in mental health for black women in particular?
DONNA: I want to start by just echoing what you said. So, we know that black and brown communities are disproportionately impacted by healthcare disparities, and I think if nothing else, covid illuminated that our members who are in medical assistance face many disparities just due to their address or their geography and some of the barriers, like we talked about, education, transportation, childcare, food, all of those things. I can tell you that over 30% of our eligible members reside in North Philly, the lower northeast, Southwest and West Philadelphia, and we know that those are high need communities. These communities have the lowest life expectancy and the highest rates of poverty, homicide, infant mortality, drug overdose, all of those things. And 2022 of our membership, 75% identified as black or Hispanic. And so, that just gives you some grounding in terms of who our members are. 11% use a primary language other than English. And so, it's incumbent upon us, as the managed care organization, to really infuse a health equity lens, a DEI lens, through all of the work that we do. And we've done that in a number of ways. One, we just polished off our three year strategic plan. And so, the three main pillars are a people first culture, and that's for our members and our staff, whole person care. We've been talking a lot about that, particularly through our community-based care management and driving organizational excellence, being efficient, driving quality, being good fiscal stewards. All of this work has been infused with a DEI perspective. One of the things that we really committed to back in 2022 was obtaining a multicultural healthcare distinction. And we did, and that's an accreditation that's awarded by the National Committee for Quality Assurance. It's a gold standard in healthcare. So, we got that, and right now we are preparing for NCQA healthcare equity accreditation, which is similar, but a little bit more robust, and generally speaking, we also, have NCQAs Managed Care accreditation. These processes are really vigorous, and they cover everything from your policies and procedures and your hiring practices to your network capacity and your network demographics. So, it really forces you to look at where you potentially have some gaps and address those. And now in 2025 we're going to be going after health equity accreditation. And why that's important is because the rigors of obtaining those. Accreditations really force the organization and everything that it does, from its policies, procedures, its hiring, its recruiting, the composition of its provider network, to really have DEI and health equity infused across all of those things. So, I think it's really important to start with how we function as an organization being the basis through which we are going to address health care disparities, particularly for black women and black parenting and postpartum women in particular. So, we've done that work, and are continuing to do that work. We're also, working with our provider network, because they are the people who are actually directly interfacing with members. We are requiring all of them to train their staff and cultural competency, and that's going to be a lift. We'll have some conversations about timelines and how we can support that. We also, think that's a very important investment to make. We are also, really focused on meeting members where they are. We talked a little bit about that through some of the care management strategies, but you also, have an initiative that we're kicking off in July that we're really excited about. It's called the hair initiative, and that stands for Health Access Initiative for Recovery. And what we're doing with this pilot is we are training up barbers and stylists in the north Philadelphia zip code, where we've seen a spike in overdoses. We're training those stylists and barbers on how to talk to their clients about mental health, about depression, about anxiety, about, you know, my child is experiencing this, and so, we're going to train them and some key components of how to have those conversations in a trauma-informed way. We're going to equip them with resources. They'll have our Member Services number which I have to put a plug in for. One 888, 545, 2600 operates 24 hours a day, seven days a week. We see stylists and barbers as a really important component of the Black and African American community, and so, it's a way that we're really trying to partner, get folks trained up and be able to have those conversations in a way that's less diagnostic and less stigmatizing and more welcoming and just coming from a space of relationships. You know, people have relationships with their barbers and stylists, so, we're starting it off as a pilot, but we're hoping to scale that up throughout Philadelphia. I think that's important to say, not everybody needs treatment, but we all need a touch point on how we're feeling and how we're doing, and if we need some additional assistance in something which who doesn't from time to time.
SARAH: You know the innovation that you're describing right now lends insight, even in terms of how we talk about workforce, this idea, we really are all in it together, and there are so, many ways that we need to be addressing the mental health of a community, through prevention, through treatment, but we also, know that many provider organizations have been struggling to retain their workforce, and this is certainly not limited even to the mental health profession. We see that in childcare. Certainly, see it in nursing. So, how has that been looking in Philadelphia? Are you seeing any promising strategies to support it? What are your thoughts on our workforce challenges?
DONNA: Yeah, yeah, it's really challenging. And I think that specifically for the behavioral health sector, we've seen people leave the field altogether. It is extremely hard to hire a psychiatrist right now and forget about finding a child psychiatrist. We've seen direct care staff leave the field and go work in retail or some other space. And so, it's pretty dire, and it's one of the reasons that we're hearing from providers that their businesses are being really impacted, and it's impacting access. If you don't have staff, you can't deliver the service. And everybody's feeling it across the board. And as you said, across sectors, I think in a city of EDs and meds, it's really incumbent upon us to think about this strategically and for the long term. You know, I wish there were some quick, easy answers, but I think that this is a long haul strategy, starting with really professionalizing the work for direct care staff, in particular, these are often the lowest paid people who are doing the heavy lift and who have their own trauma and are potentially experiencing trauma through the work that they're doing with the people they're supporting. And so, professionalizing the work, embedding in supports for health and wellness of the staff. And then I think, How can we look at what's actually needed for a particular position? We have these conversations here at CBH all the time. I'll look at a job description, and we're asking for five levels of credentialing, and maybe we only need two. And so, I think it's taking a step back. We never want to compromise quality. Right? But I think we need to think differently. You know, maybe there's opportunities for somebody who is new out of school to do their training and still work, you know, and gain those supervision hours, why they're actually working, you know, looking at growing the pipeline through internships and partnerships with the schools, and I think providers working together. You know, sharing staff is not something that we typically think about doing, but is that something that could work? I think it's longer term, but I definitely think it's the time where we need to sit down and really start coming up with some concrete next steps.
SARAH: So, this could be related to workforce, but certainly related to any of the issues that you've talked about. Are there things that you're looking to government to support, whether that's at the state level, federal level, what kinds of systems change could help support some of the promising practices that you've been describing?
DONNA: So, I again have to give a shout out to our partners at the state in particular, Pennsylvania Department of Human Services, or PA DHS, they recently submitted what's called an 1115 waiver. It's called bridges to success, keystones of health for Pennsylvania. And what that would do is allow for Medicaid to pay for things that address the social determinants of health. Right now, we pay for treatment, but this waiver would allow Medicaid-managed care organizations to pay for child care, to pay for services for people when they're what we call behind the walls. So, when people get incarcerated, their coverage stops, but this would allow for that coverage to continue and for transition planning post-incarceration, it would pay for food. It could potentially pay for continuous coverage for kids. So, we are really excited. We've done a letter of support. We believe that this will ultimately be approved by CMS. I think what we're very interested in understanding is the logistics and how it gets operationalized. And so, even in our regular business, we often see some of the smaller agencies really struggle with the rigors of Medicaid billing and the infrastructure around that. So, I think we're very curious to understand how the federal government and the state government will support those communities organizations or provide pass through organizations to help them with the Medicaid side of it. So, we're super excited about this. This is a game changer.
SARAH: So, Donna, as we had talked before, I mean, you really only been back eight months, not even a year. What are you most excited about? Obviously, the Medicaid waivers coming through would be an incredible opportunity for the state. What's exciting you know, for your team at CBH, for things on the horizon in Philadelphia,
DONNA: I'm really super excited that I'm not managing through the pandemic. The last time I did this, it was covid all day, every day, and so, to come back where we're not in crisis mode has really been nice, and I can actually engage with staff directly and not on Zoom every day. So, just from a personal and professional perspective, it's nice to be back at 801 and to see people and have all staff meetings and do things that are fun and encouraging for our team, we have an incredibly talented, dedicated group of people I work with the best leadership team ever, aside from my colleagues at PHMC. It's been really nice being back and being in this work that I think is so, impactful right now in this moment where we are but I think things like the hair project, working with partners to come up with other really innovative things that are not a heavy lift and are not a big financial spend, and people already have ideas. And so, one of the things we're trying to do is not have this be a top down organization, but really encouraging creativity and innovation across the organization. One of the other things I'm excited about are some of the changes that are happening within city government. So, right now, many of the commissioners are acting or interim, and so, there'll be people who will be remaining in those positions. It's always really exciting time to see what the vision at the higher level is going to be and what role CBH can play in having that vision materialized. So, really excited about that as well. Another thing that I would just flag is that we don't do this work in a vacuum. There are other managed care organizations across the Commonwealth that we have really strong partnerships with, and so, we can pick up the phone anytime and say, this is happening in Philly. What are you seeing? Or you did this program? We're thinking about standing it up here. And the hair project was actually one that was started by Community Care Behavioral Health, and so, they really partnered with us. We're using the consultant that they used. So, really excited about those things, but I think overall, what excites me most is having the opportunity to. Work with the team here to have CBH be the best managed care company we can be all of those metrics that we're measured on. I want us to have really excelled in those areas, because ultimately what that means is good quality, accessible care for our members. We have a lot of different metrics that could make your eyes glaze over, but ultimately, when we do well, that means things are happening well out there on the front line.
SARAH: This has been such a fantastic conversation. Thank you so, much for making time to share your expertise, and really, I'm just excited to see where things go from here.
DONNA: Thank you so, much for having me. It's always so, good to talk with you, and I just appreciate the opportunity to talk about all the good things that we're doing here in Philadelphia and at CBH and within our provider network. So, thank you.
SARAH: Thanks again to Donna for making time for this conversation. Thank you also, to the van Ameringen Foundation for your support to help raise awareness around access to mental health services. You can find our most current and past episodes of at the core of care, wherever you get your podcasts, or at pactioncoalition.org on social media. You can stay up to date with us through our handle @paaction and @nurseledcare. This episode of At the Core of Care was produced by Emily Previti of Kouvenda Media and mixed by Brad Linder. I'm Sarah Hexham Hubbard with the National Nurse-Led Care Consortium. Thanks for joining us.

We are excited to announce that as an outcome of the thorough strategic planning process that we engaged in over the past several months, we have a new 5-year strategic plan and we will be refreshing our brand as the Pennsylvania Nursing Workforce Coalition (PA-NWC).
When we embarked on this process, our goals were to:
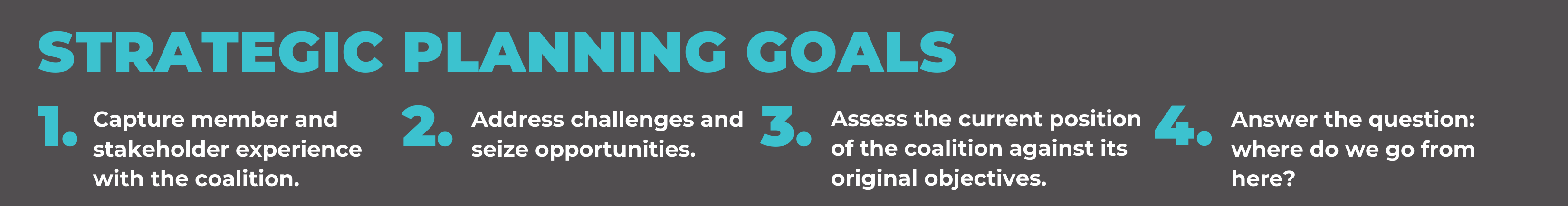
In the summer of 2023 we hired Generative Consulting Partners to guide us and we created several opportunities for engagement from our Advisory Board and stakeholder base. This included a survey, virtual focus groups, visioning sessions, and in-person meetings. Please find a synopsis of the feedback below:
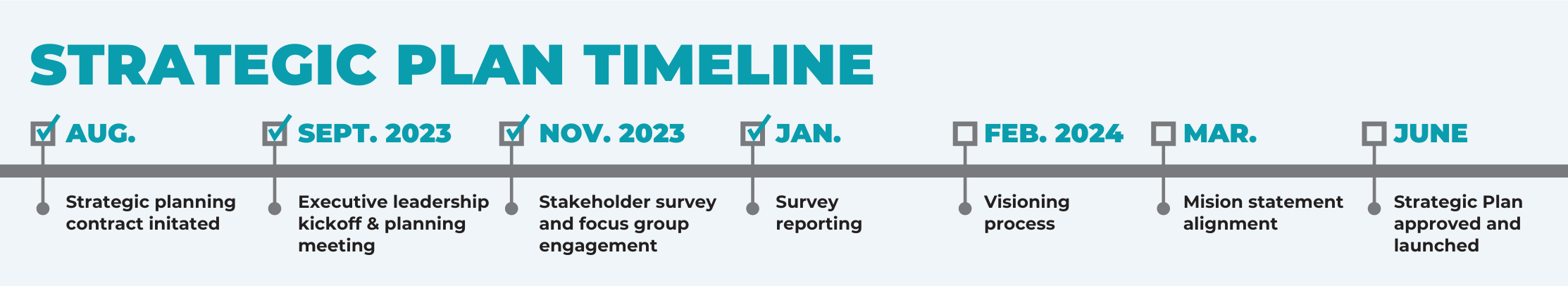
Through this thorough review, it became clear that it would be beneficial to clarify our external role to new and existing stakeholders and to strengthen our position as Pennsylvania’s Nursing Workforce Center. Our feedback expressed that one of our core strengths was our anchor in the national framework of the Future of Nursing’s goals and that our participants continue to feel connected to and inspired by its principles, and there was an increased desire for communications and advocacy efforts. So in approaching our strategic plan, it was imperative to maintain this connection to the Future of Nursing, but we felt it would be helpful for our name to be more reflective of the work that we do to allow us to evolve and expand our external presence.
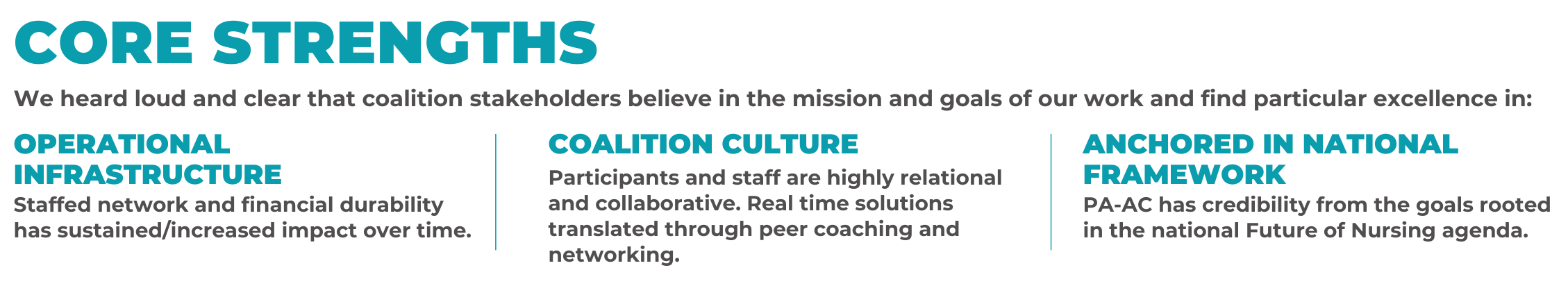
We are therefore thrilled to announce that effective June 17, 2024, we will be referring to ourselves as the Pennsylvania Nursing Workforce Coalition (PA-NWC) to honor our roots and our future.
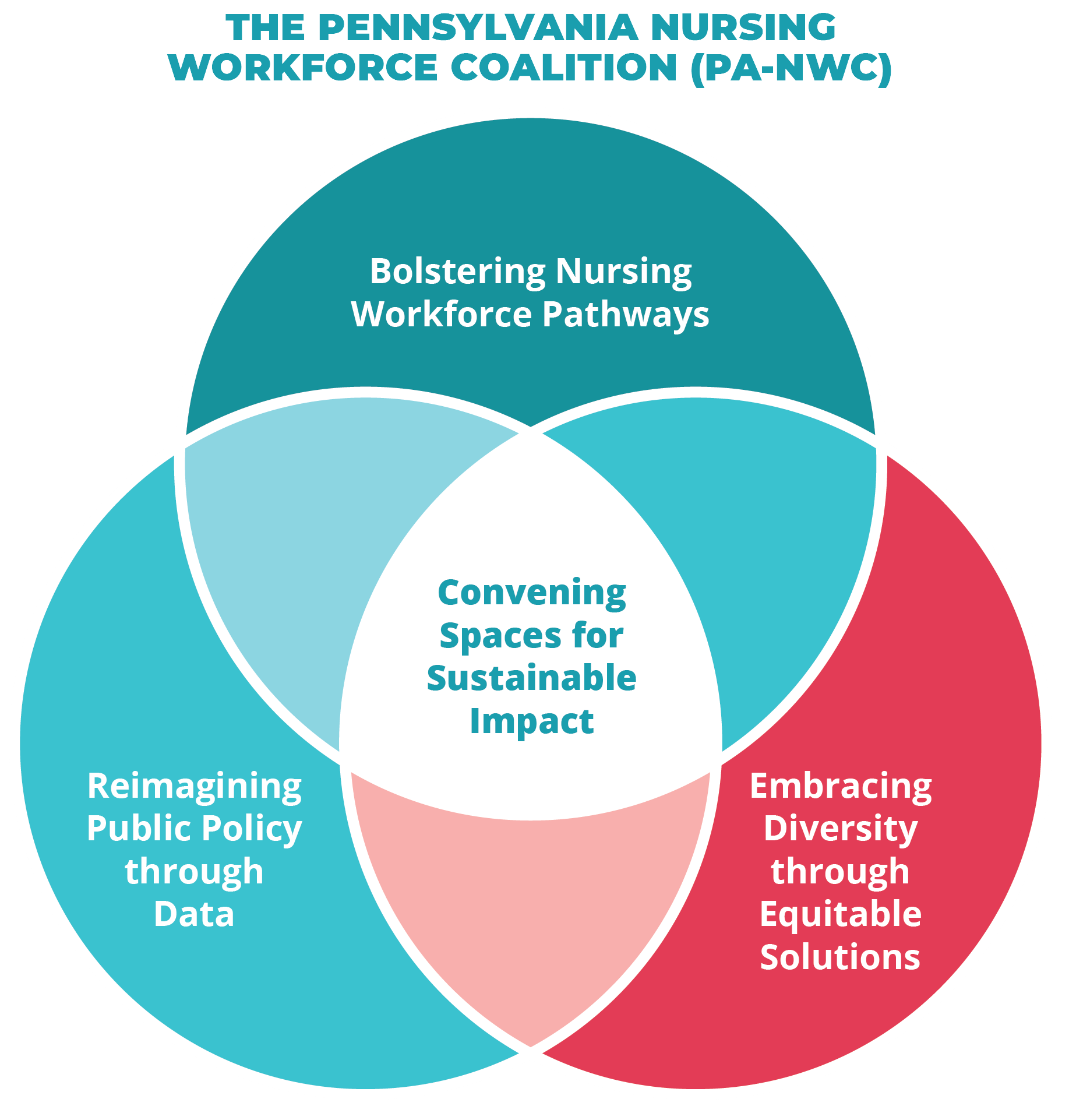
OUR VISION: A healthy Pennsylvania through equitable, high quality, and safe nursing.
OUR MISSION: Advancing a nursing workforce that will lead healthcare transformation by cultivating strategic partnerships with diverse populations and organizations.
We are calling this a “brand refresh” and not a “rebrand” because we want to be clear that the components of our structure are not changing.
The PA-NWC will continue to function as a program of the National Nurse-Led Care Consortium (NNCC), operating under the terms of NNCC’s Bylaws, as a Pennsylvania nonprofit corporation, and as a 501(c)(3) tax-exempt organization.
Further, we will maintain our Advisory Board structure as a coalition with organizations as members and individual representatives.
The Pennsylvania Action Coalition has “housed” the Pennsylvania Nursing Workforce Center since 2016. The “brand refresh” is just making this work more front and center.
We also want to iterate that the PA-NWC is not distancing itself from the Future of Nursing reports nor the Campaign for Action.
Many other nursing workforce centers across the country are simultaneously their own state’s Action Coalition and workforce center and present themselves as their state’s nursing workforce entity if they are not housed within a school of nursing.
Details about our new strategic plan:
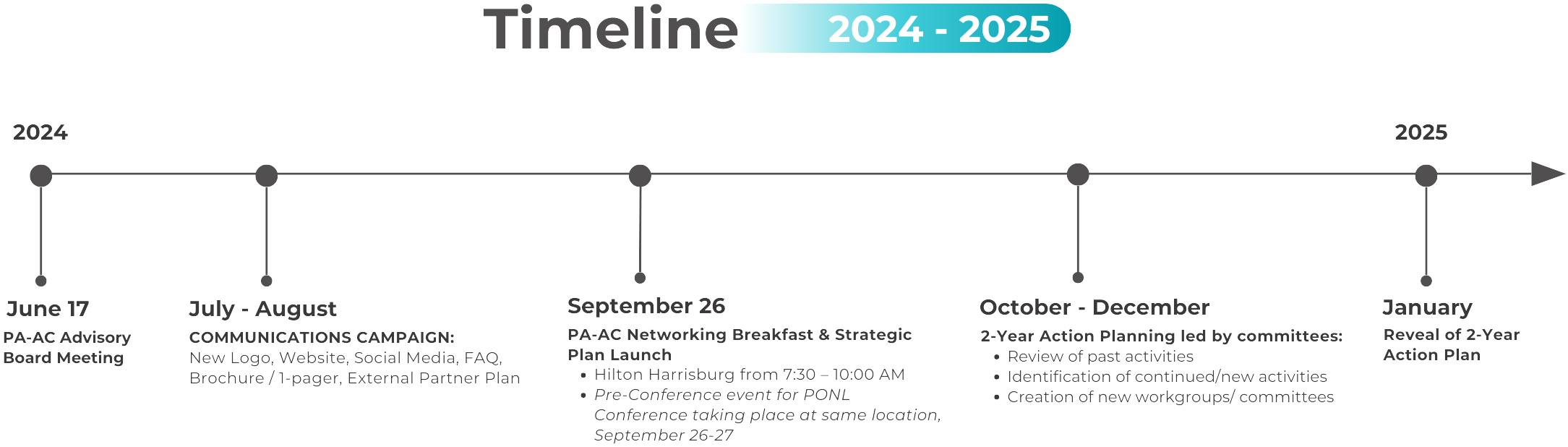
With regards to our implementation plans, we are in the midst of building a communications campaign this summer for our internal and external stakeholders. We plan to develop the following as part of this campaign with a goal of September 26 being our first formal external in-person reveal of our new plan and name:
On September 26, 2024, the Pennsylvania Nursing Workforce Coalition (formerly known as the Pennsylvania Action Coalition) we hosted a successful and engaging breakfast at the 2024 Pennsylvania Organization of Nurse Leaders (PONL) Annual Leadership Conference in Harrisburg, PA. The pre-conference event marked the unveiling of the PA Nursing Workforce Coalition’s (PA-NWC) new strategic plan and the introduction of its key initiatives, aimed at advancing the nursing profession in the state. The breakfast event featured a presentation from our team about the PA-NWC’s new strategic direction. Check out the event recap below!

The Pennsylvania Nursing Workforce Coalition's mission is to advance a nursing workforce that will lead healthcare transformation by cultivating strategic partnerships with diverse populations and organizations.
Partnerships with stakeholders and volunteers allow us to implement initiatives that strengthen the nursing workforce. Your involvement and support allows us to advance nursing to help transform health and health care.